Moneypox Data?
So far, the available data regarding moneypox is vague, incomplete and contradictory. The world deserves access to accurate, up-to-date, coherent and complete data regarding the "moneypox" PHEIC.
The data that is publicly available regarding moneypox (Mpox) clearly conflicts with many statements that have been made by public officials and organizations.
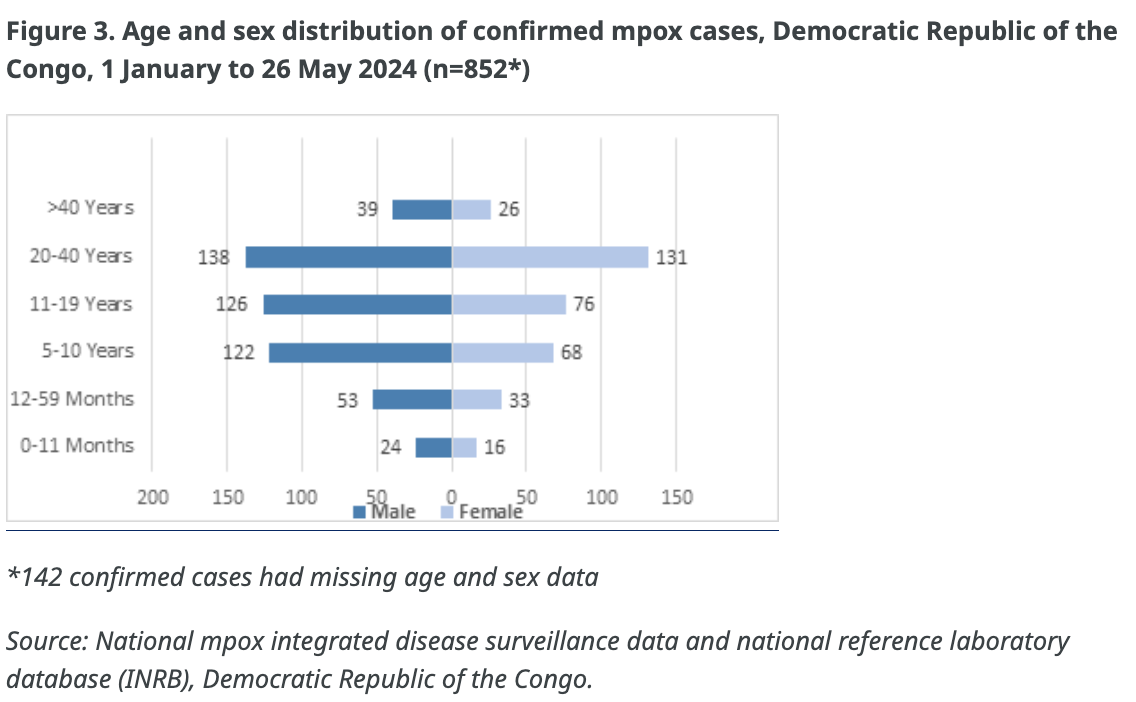
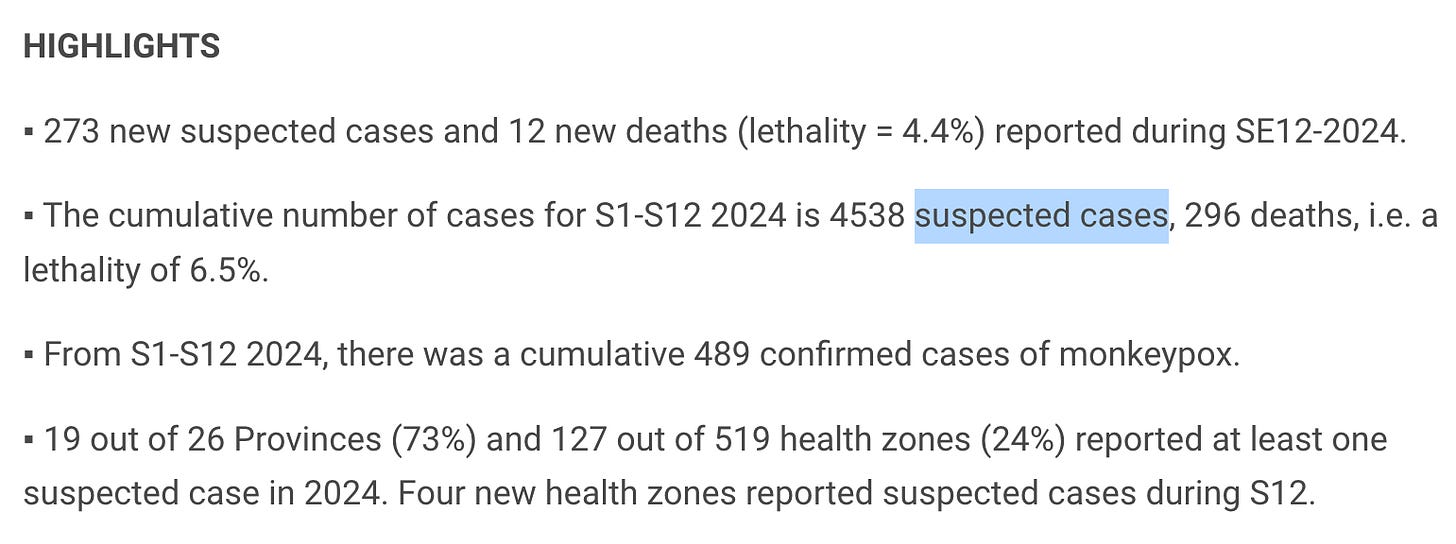
The problem appears to be that some of the available data refers to “confirmed” cases, some of the data refers to “probable” cases and some of the data refers to “reported” or “suspected” cases. (see CDC definitions)
Also, the data regarding the new “Clade 1b” has not been adequately detailed.
Will any valid, up-to-date, complete, coherent and accurate data ever be made available?
What is the truth?
If anyone has access to newer or more accurate and complete data, please post it in the comment section below:
The data below is from the Africa CDC:
August 13, 2024
At least 12 African countries, including previously unaffected nations like Burundi, Kenya, Rwanda, and Uganda, have reported Mpox outbreaks. So far in 2024, these countries have confirmed 2,863 cases and 517 deaths, primarily in the Democratic Republic of the Congo (DRC). Suspected cases across the continent have surged past 17,000.
and also this information:
July 30, 2024
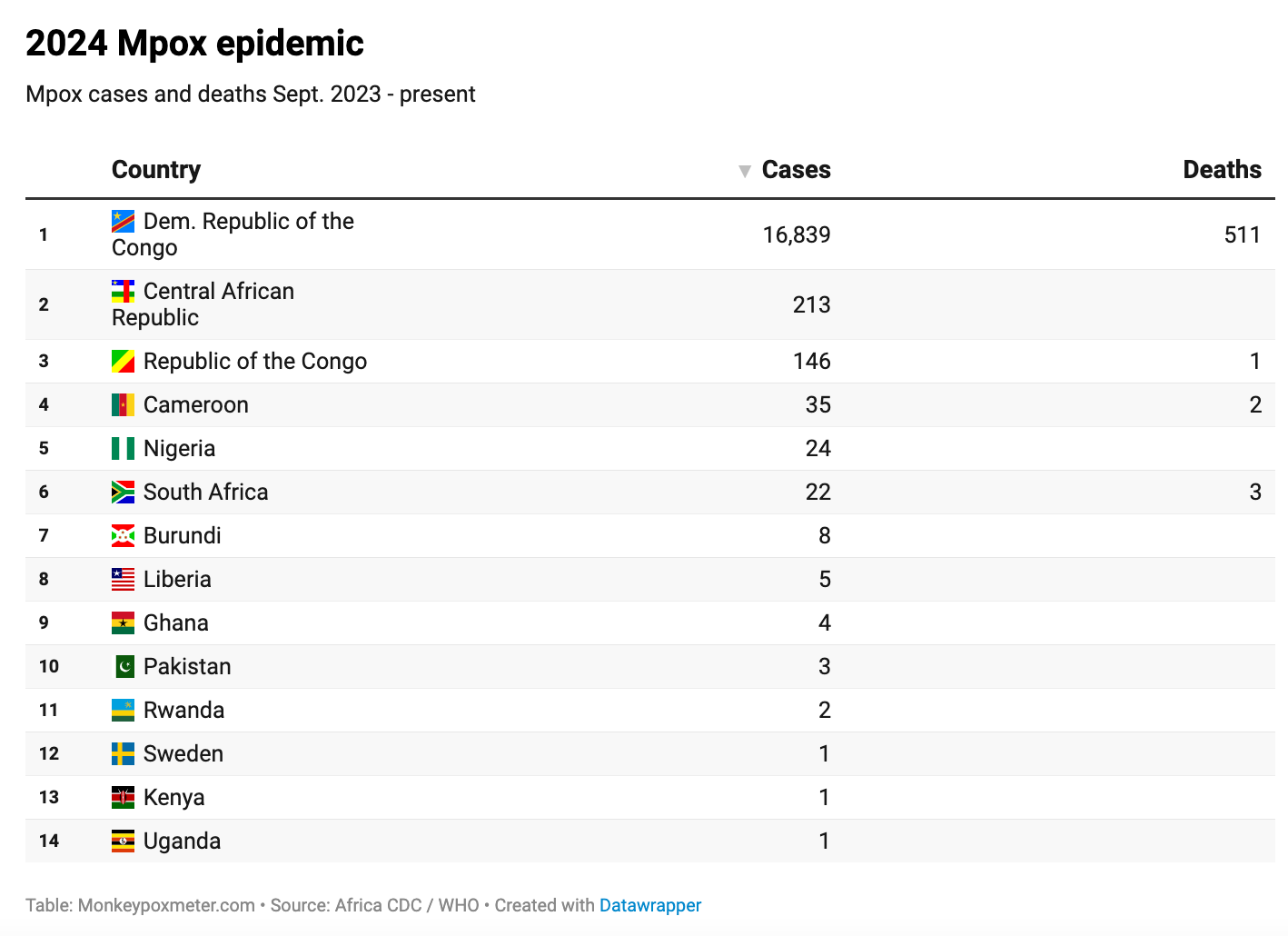
Since the beginning of this year and as of July 28, 2024 a total of 14,250 cases (2,745 confirmed; 11,505 suspected) and 456 deaths (CFR: 3.2%) of mpox have been reported from 10 AU MS: Burundi (8 cases; 0 deaths), Cameroon (35; 2), CAR (213; 0), Congo (146; 1), DRC (13,791; 450), Ghana (4; 0), Liberia (5; 0), Nigeria (24; 0), Rwanda (2; 0) and South Africa (22; 3). This represents a 160% and 19% increase in cases and deaths, respectively, in 2024 compared to the same period in 2023.
DRC accounts for 96.3% of all cases and 97% of all deaths reported this year. In addition, Chad has reported 24 suspected cases and no confirmed cases this year.
The data below is from Reuters:
August 16, 2024
There have been 27,000 cases and more than 1,100 deaths, mainly among children, in Congo since the current outbreak began in January 2023.
The data below is from the United States CDC:
August 15, 2024
Since January 2023, the Democratic Republic of the Congo (DRC) has reported more than 22,000 suspect mpox cases and more than 1,200 deaths.
The data below is from The European Centre for Disease Prevention and Control:
August 16, 2024
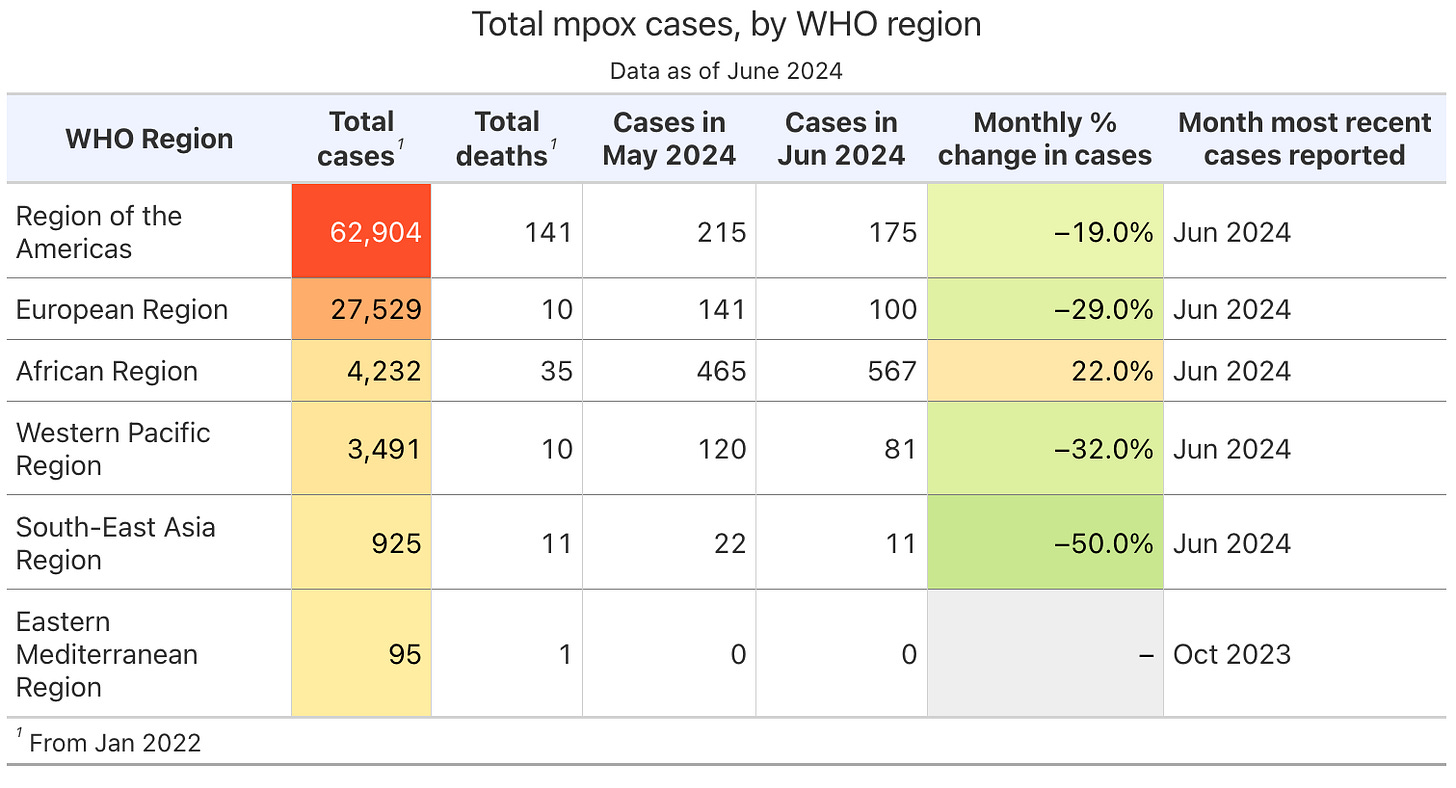
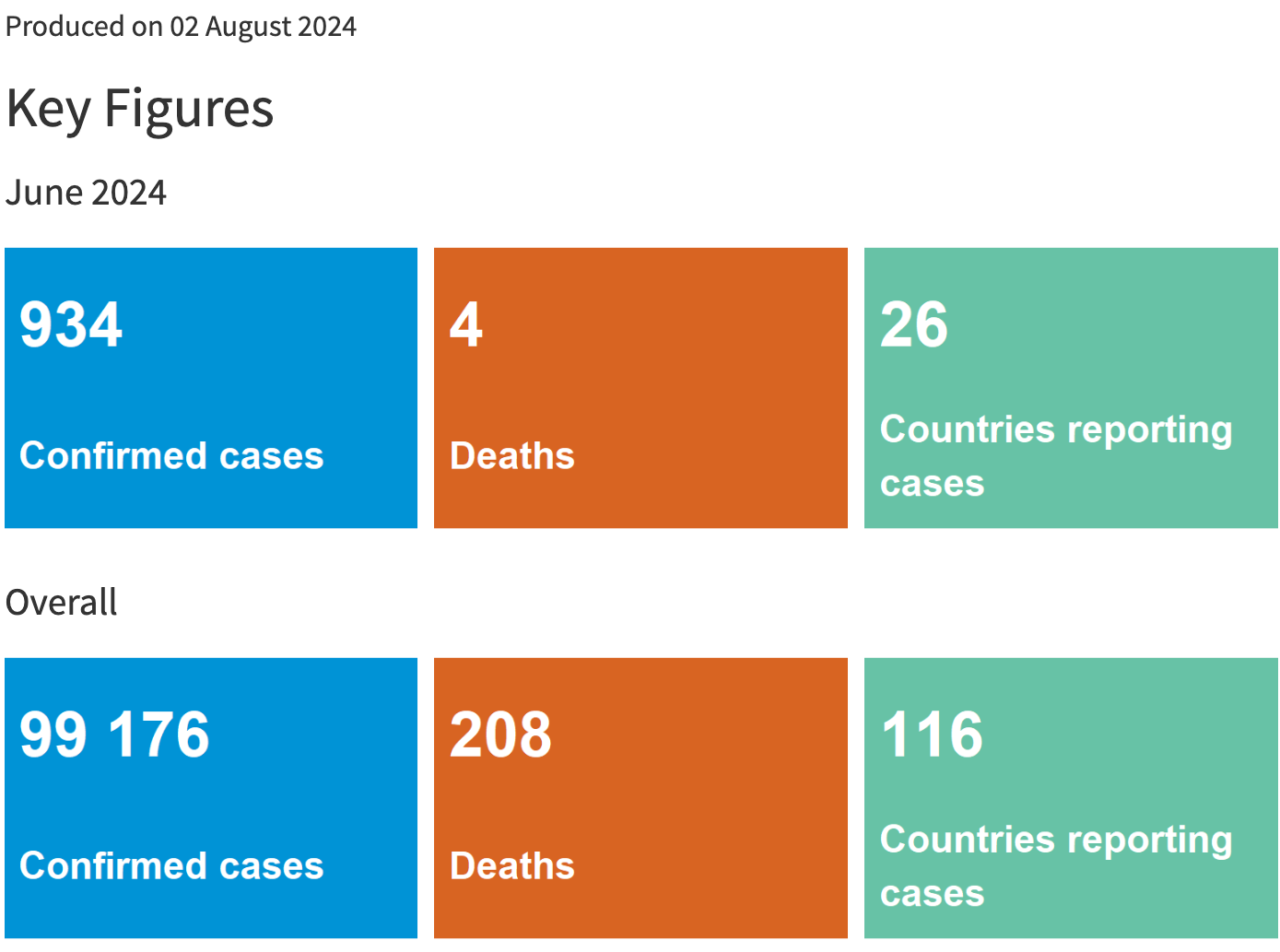
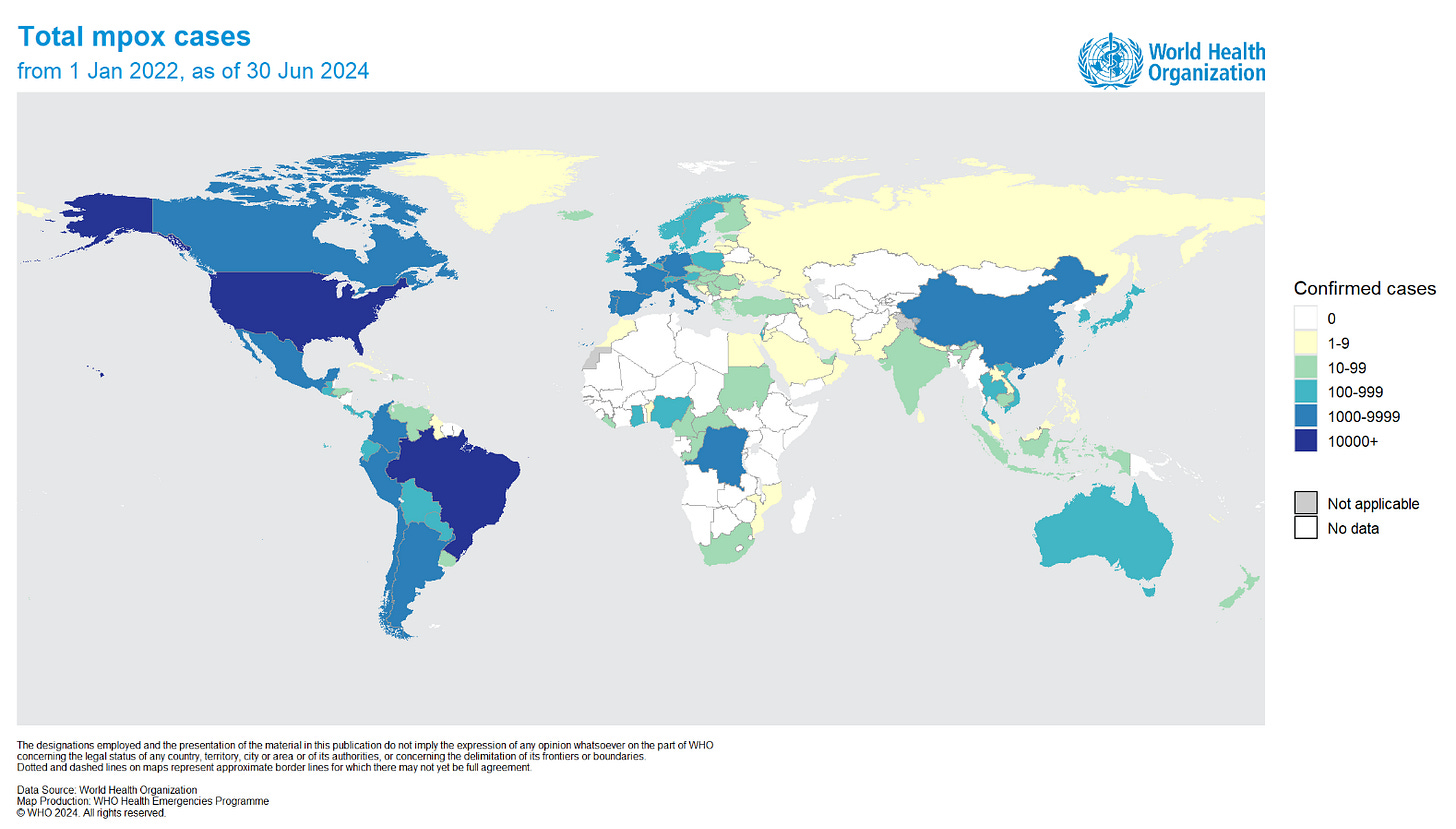
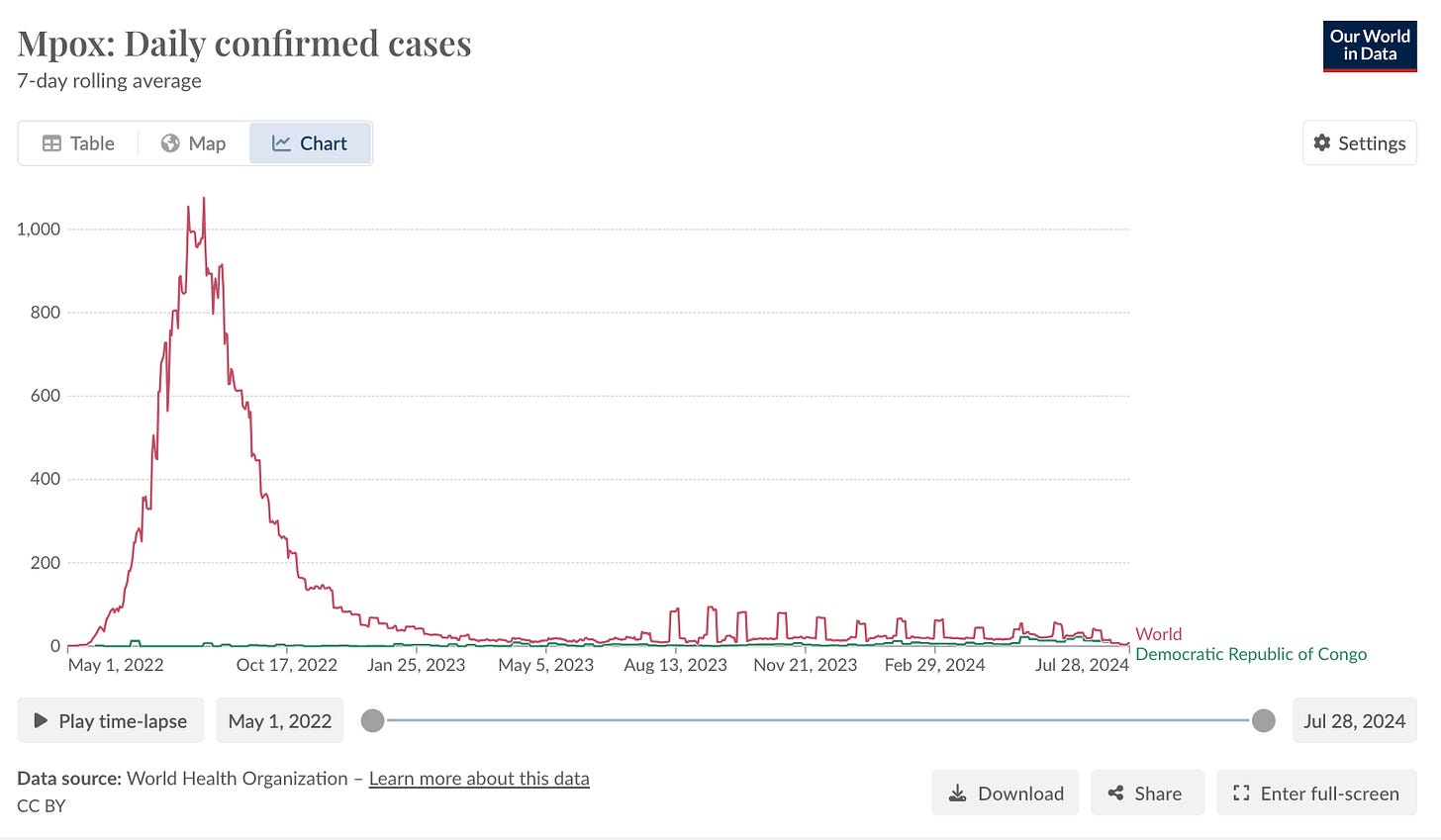
Since the beginning of the global mpox outbreak in 2022 and until the end of July 2024, 99,176 confirmed cases of mpox, including 208 deaths, had been reported by 116 countries.
In 2024, 14,719 suspected and 2,822 confirmed mpox cases (total 17,541) have been reported in the African continent, including 517 deaths (case fatality 3%), according to the Africa Centres for Disease Control and Prevention (Africa CDC).
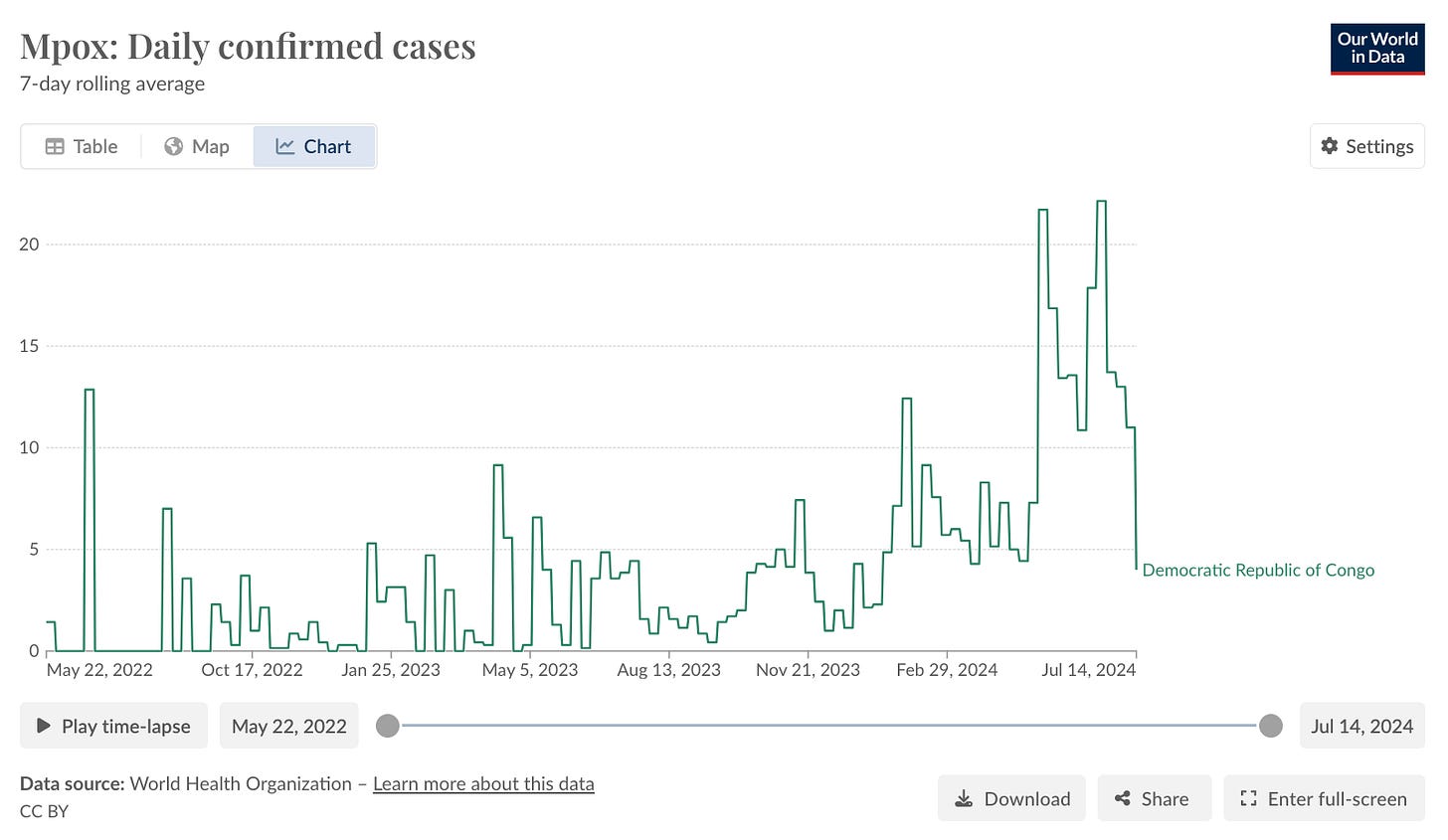
In 2024, DRC has reported 16 789 cases (14 151 suspected and 2 638 confirmed) including 511 deaths (case fatality 3%) from all of the country’s provinces, representing the highest number of cases due to clade I in Africa.
Confirmed mpox cases have also been reported in five of the eight neighbouring countries to DRC in 2024, i.e.
Burundi (61 confirmed, 165 suspected),
Central African Republic (35 confirmed, 223 suspected),
Congo (19 confirmed, 150 suspected),
Rwanda (four confirmed), and
Uganda (two confirmed).
MPVX clade Ib, which was detected first in DRC and reported in April 2024, was also detected in confirmed cases in Burundi, Rwanda, Uganda and Kenya.
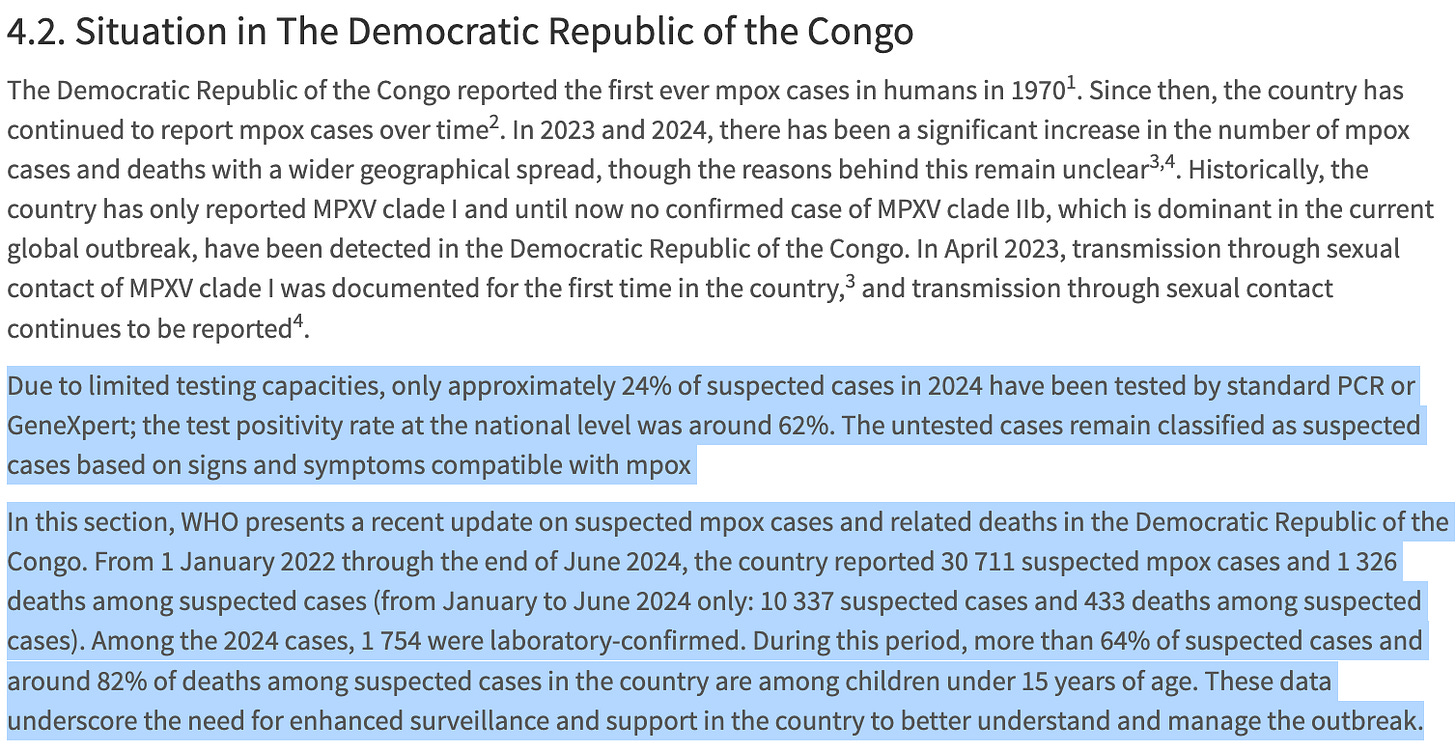
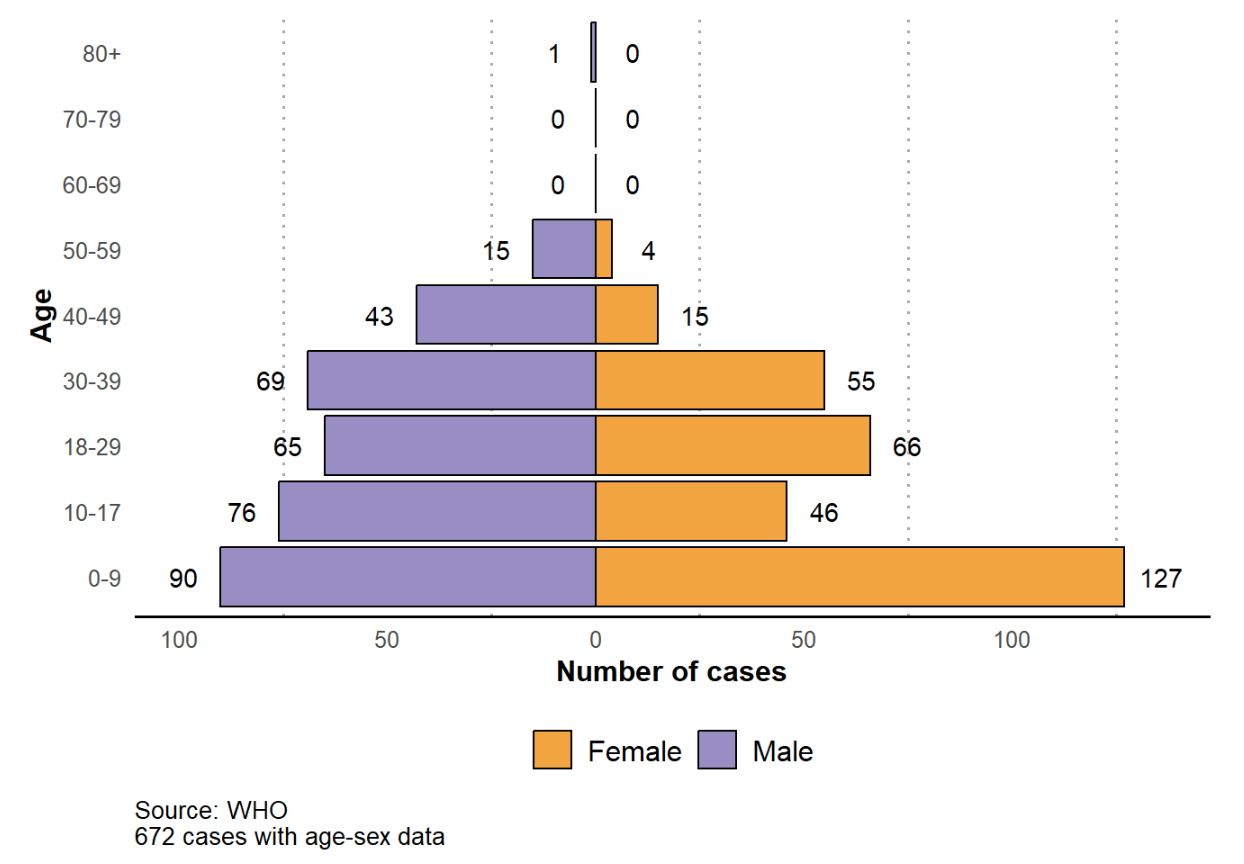
In DRC, most cases and deaths reported are among <15-year-olds, representing 66% of the total cases and 82% of the total deaths. Males account for 73% of the cases in DRC.
The data below is from the World Health Organization:
https://worldhealthorg.shinyapps.io/mpx_global/
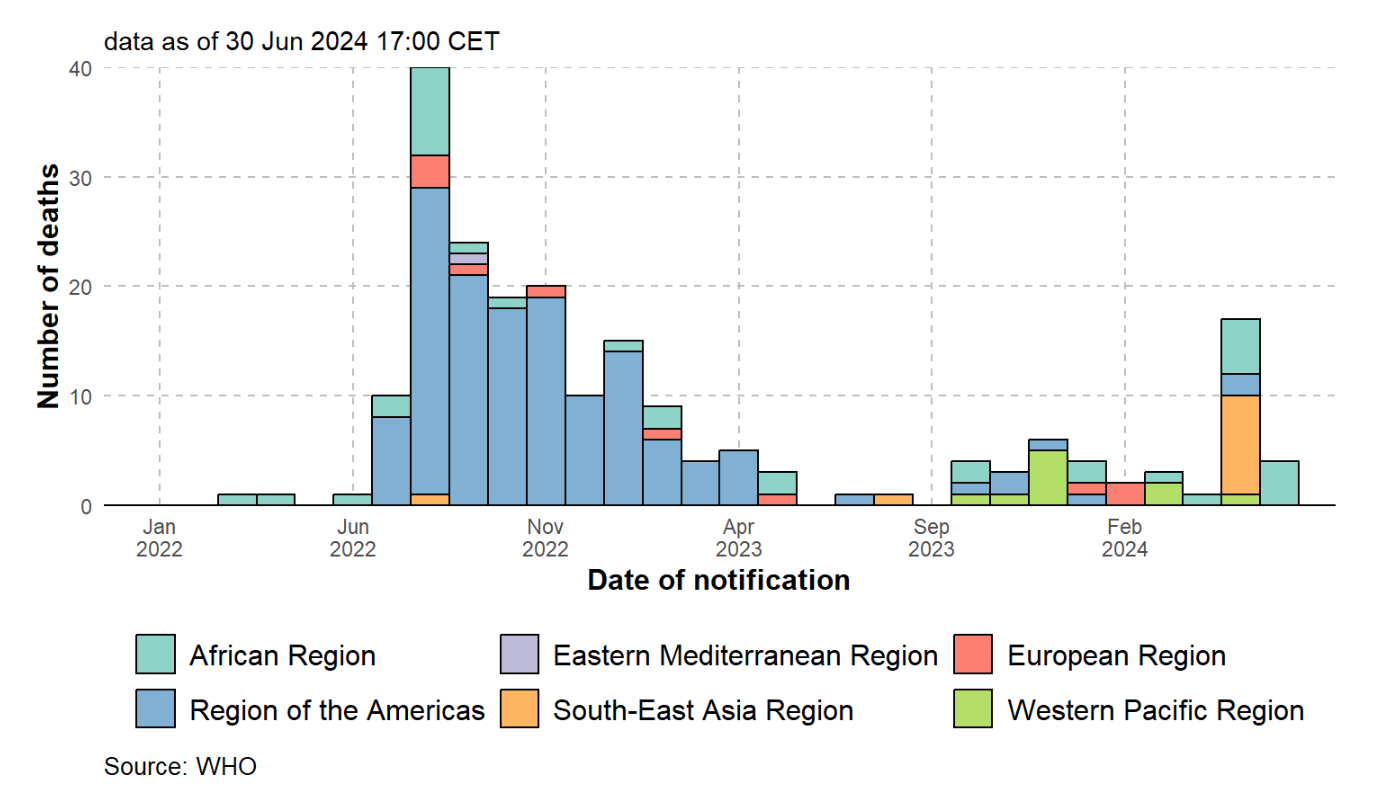
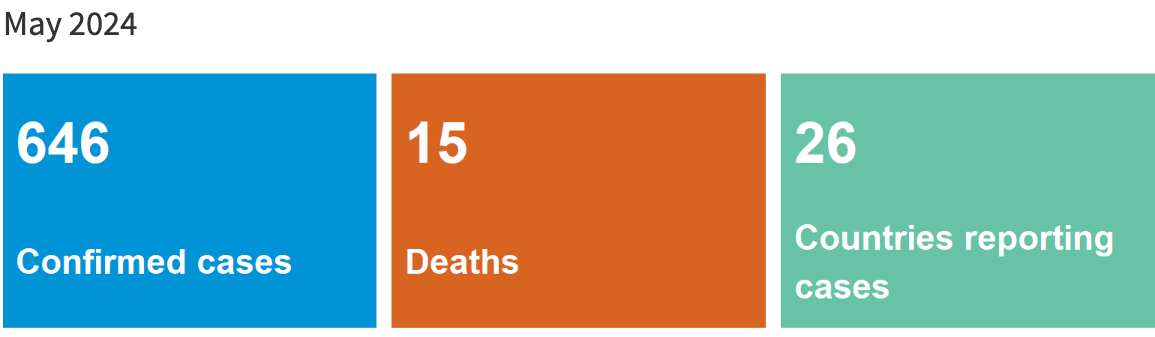
Deaths (Global)
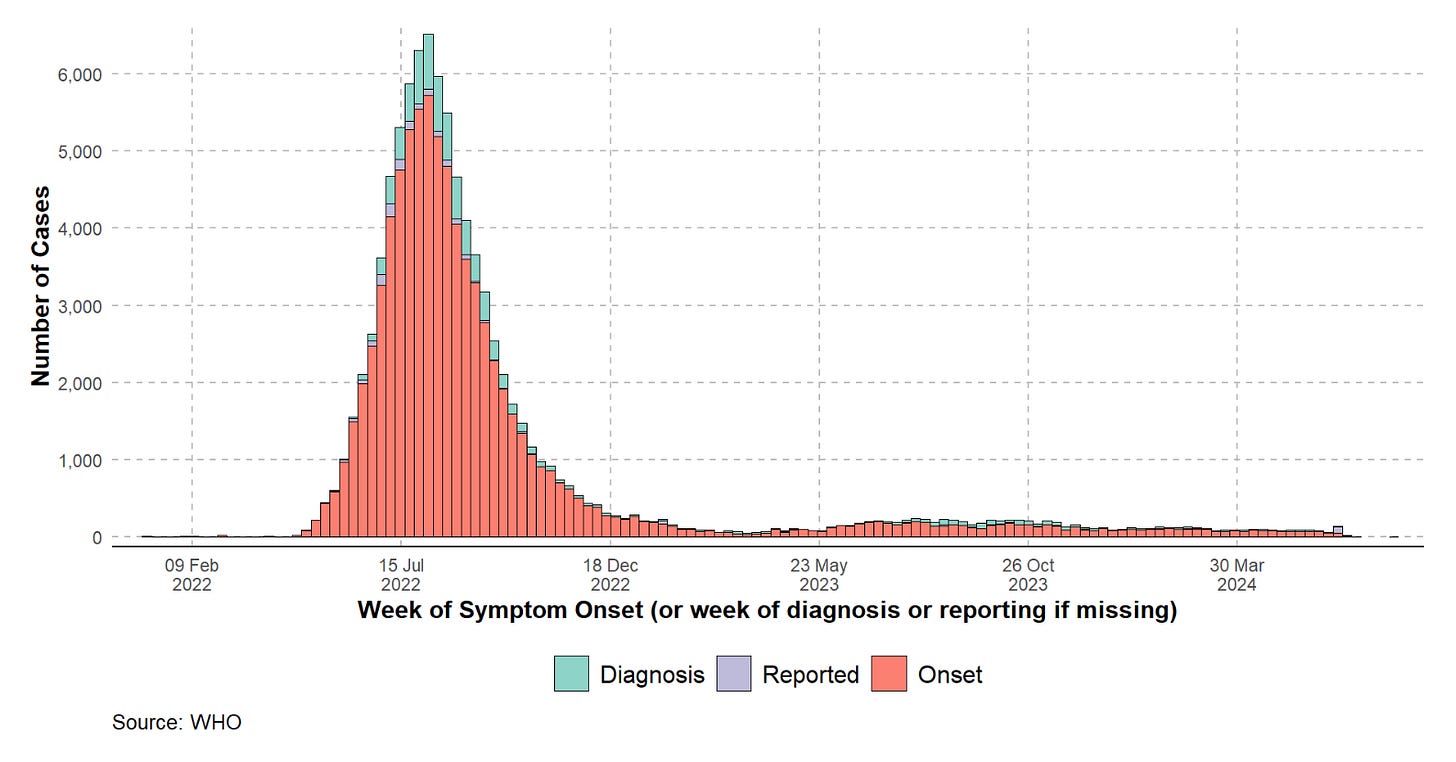
Cases (Global)
https://web.archive.org/web/20240502135635/https://worldhealthorg.shinyapps.io/mpx_global/
https://web.archive.org/web/20240527225740/https://worldhealthorg.shinyapps.io/mpx_global/
https://web.archive.org/web/20240626145804/https://worldhealthorg.shinyapps.io/mpx_global/
https://web.archive.org/web/20240816191015/https://worldhealthorg.shinyapps.io/mpx_global/
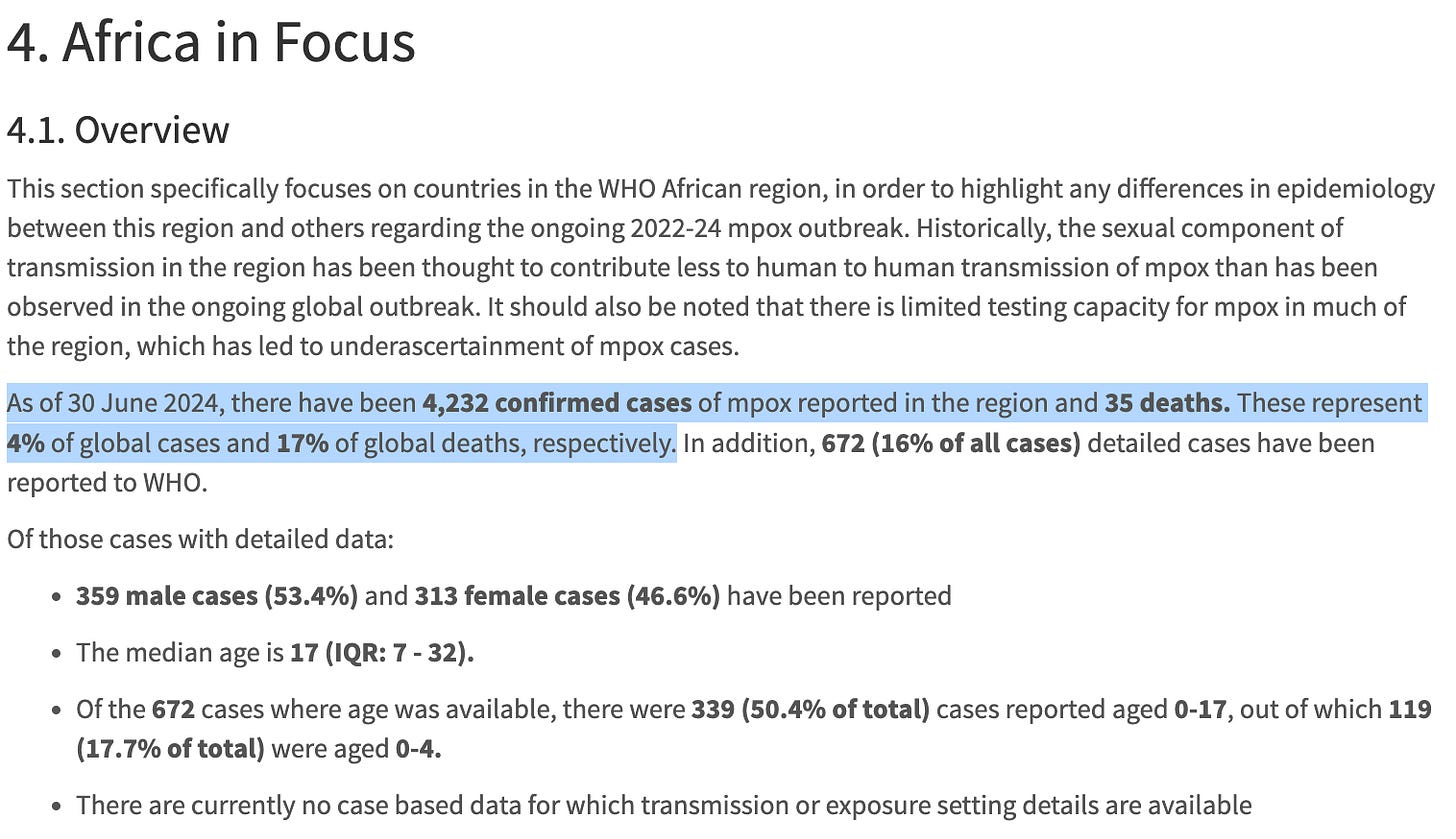
https://worldhealthorg.shinyapps.io/mpx_global/#4_Africa_in_Focus
The data below is also from the World Health Organization:
In South Kivu, between 1 January and 2 June 2024, 777 cases were reported through the national surveillance system after investigation of alerts. Following laboratory testing of samples from 426 out of 777 cases (55%), 373 cases were confirmed as positive (test positivity of 88%), including seven deaths (CFR 1.8% among confirmed cases).
https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON522
The data below is from Relief Web:
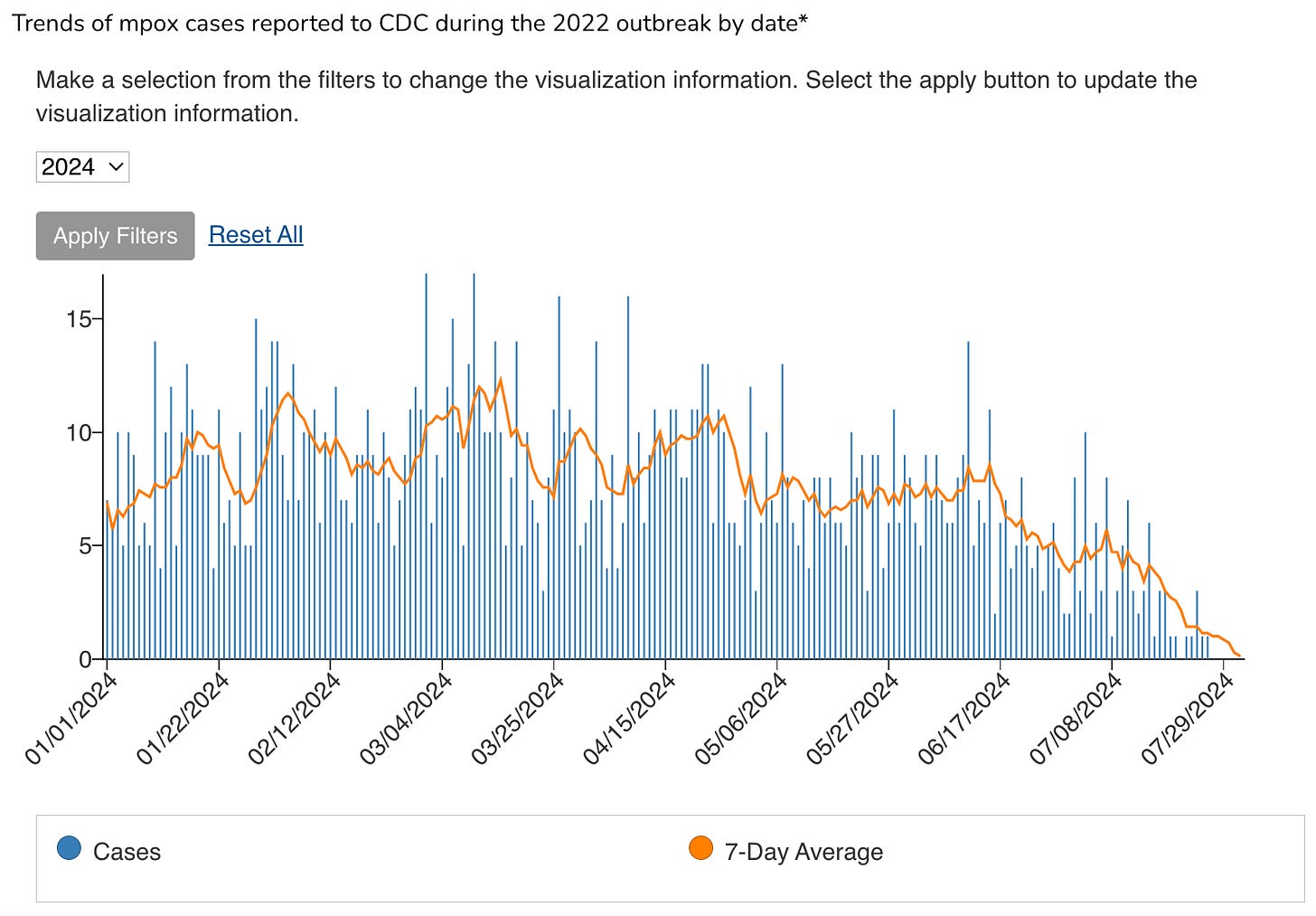
The data below is from the United States CDC:
https://www.cdc.gov/poxvirus/mpox/response/2022/mpx-trends.html
The data below is from the BBC:
Since the start of the year, there have been more than 13,700 cases of mpox in the DR Congo, with at least 450 deaths.
The data below is from Monkeypox Meter:
https://www.MonkeypoxMeter.com/
The data below is from Our World in Data:
United States CDC Mpox Case Definitions:
Updated June 10, 2024
Suspect Case
New characteristic rash* OR
Meets one of the epidemiological criteria and has a high clinical suspicion for mpox
Probable Case
No suspicion of other recent Orthopoxvirus exposure (e.g., Vaccinia virus in ACAM2000 vaccination) AND demonstration of the presence of
Orthopoxvirus DNA by polymerase chain reaction of a clinical specimen OR
Orthopoxvirus using immuno-histochemical or electron microscopy testing methods OR
Demonstration of detectable levels of anti-orthopoxvirus IgM antibody during the period of 4 to 56 days after rash onset
Confirmed Case
Demonstration of the presence of monkeypox virus (MPXV) DNA by polymerase chain reaction testing OR
Next-Generation sequencing of a clinical specimen OR
Isolation of MPXV in culture from a clinical specimen
Epidemiologic Criteria
Within 21 days of illness onset:
Reports having contact with a person or people with a similar appearing rash or who received a diagnosis of confirmed or probable mpox OR
Had close or intimate in-person contact with individuals in a social network experiencing mpox activity, this includes men who have sex with men (MSM) who meet partners through an online website, digital application (“app”), or social event (e.g., a bar or party) OR
Traveled outside the US to a country with confirmed cases of mpox or where MPXV is endemic OR
Had contact with a dead or live wild animal or exotic pet that is an African endemic species or used a product derived from such animals (e.g., game meat, creams, lotions, powders, etc.)
Exclusion Criteria
A case may be excluded as a suspect, probable, or confirmed case if:
An alternative diagnosis can fully explain the illness OR
An individual with symptoms consistent with mpox does not develop a rash within 5 days of illness onset OR
A case where high-quality specimens do not demonstrate the presence of Orthopoxvirus or MPXV or antibodies to orthopoxvirus
https://www.cdc.gov/poxvirus/mpox/clinicians/case-definition.html
Interim Case Definitions for Clade I Mpox*
As of June 10, 2024
Suspect Case, Clade I
Probable or confirmed mpox as defined above AND
At least one of the Clade I Epidemiologic Criteria (below)
Probable Case, Clade I
Probable or confirmed mpox as defined above AND
At least one of the Clade I Epidemiologic Criteria (below) AND
Clade I and clade II MPXV-negative by polymerase chain reaction testing without Next-Generation sequencing of a clinical specimen to confirm clade
Confirmed Case, Clade I
Demonstration of the presence of clade I MPXV DNA by polymerase chain reaction testing or Next-Generation sequencing of a clinical specimen
Clade I Epidemiologic Criteria
Within 21 days of illness onset:
Traveled to an area with evidence of sustained human to human transmission of clade I mpox or where clade I MPXV is endemic, OR
Reports having contact with person with confirmed, probable or suspect clade I mpox, OR
Had close or intimate in-person contact with individuals in a social network currently experiencing clade I mpox activity, OR
Had contact with a dead or live wild animal or exotic pet that is a central African endemic species or used a product derived from such animals (e.g., game meat, creams, lotions, powders, etc.)
https://www.cdc.gov/poxvirus/mpox/clinicians/case-definition.html
Laboratory Testing
The laboratory diagnosis of mpox is predominantly based on the direct demonstration of the Orthopoxvirus monkeypox (MPXV) in a clinical specimen.
Real-time polymerase chain reaction (real-time PCR) on skin lesion materials (e.g. swabs, exudate, or lesion crusts) are used most frequently.
Viral throat swabs can be used for high risk contacts of confirmed or high-probable cases who have developed systemic symptoms but do not have a rash or lesions that can be sampled.
Several real-time PCR assays for the specific detection of MPXV, or for generic orthopoxvirus detection are available [31-36].
Over 80 MPXV laboratory tests are CE-validated, mostly based on PCR [31-36].
31. Maksyutov RA, Gavrilova EV, Shchelkunov SN. Species-specific differentiation of variola, monkeypox, and varicella-zoster viruses by multiplex real-time PCR assay. Journal of Virological Methods. 2016;236:215-20. Available at: https://www.sciencedirect.com/science/article/pii/S0166093416300672
32. Li Y, Zhao H, Wilkins K, Hughes C, Damon IK. Real-time PCR assays for the specific detection of monkeypox virus West African and Congo Basin strain DNA. Journal of Virological Methods. 2010;169(1):223-7. Available at: https://www.sciencedirect.com/science/article/pii/S0166093410002545
33. Li Y, Olson VA, Laue T, Laker MT, Damon IK. Detection of monkeypox virus with real-time PCR assays. Journal of Clinical Virology. 2006;36(3):194-203. Available at: https://www.sciencedirect.com/science/article/pii/S1386653206001223
34. Schroeder K, Nitsche A. Multicolour, multiplex real-time PCR assay for the detection of human-pathogenic poxviruses. Molecular and Cellular Probes. 2010;24(2):110-3. Available at: https://www.sciencedirect.com/science/article/pii/S0890850809000772
35. Luciani L, Inchauste L, Ferraris O, Charrel R, Nougairède A, Piorkowski G, et al. A novel and sensitive real-time PCR system for universal detection of poxviruses. Scientific Reports. 2021;11(1):1798. Available at: https://www.nature.com/articles/s41598-021-81376-4
36. Li D, Wilkins K, McCollum AM, Osadebe L, Kabamba J, Nguete B, et al. Evaluation of the GeneXpert for human monkeypox diagnosis. The American Journal of Tropical Medicine and Hygiene. 2017;96(2):405. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5303045/
Sources:
https://worldhealthorg.shinyapps.io/mpx_global/
https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON522
https://www.cdc.gov/poxvirus/mpox/response/2022/mpx-trends.html
https://www.monkeypoxmeter.com/
https://ourworldindata.org/mpox
James Roguski
310-619-3055
JamesRoguski.substack.com/archive
All content is free to all readers.
All support is deeply appreciated.






















I cannot believe the data. I mean, some of it may be accurate but look at the sources. They are just ginning up the fear factor narrative to drive participation in the forthcoming “vaccine”.
I pulled this from The World Council for Health’s recent post on Mpox:
“Symptoms of monkeypox infection are usually mild and include fever, rash and swollen lymph nodes, and occasionally intense headache, back pain, muscle aches, lack of energy and skin eruptions that can cause painful lesions, scabs or crusts. It is important to note that severe cases usually have an underlying pathology – that is, the infected person has existing health issues. According to the World Economic Forum, human-to-human transmission is limited and the virus is transmitted through direct contact with bodily fluids or skin lesions, as well as indirect contact with lesion materials through items such as contaminated bedding or clothing.
In 2022 overall, 98% of infected people were gay or bisexual men, 75% were white, and 41% had human immunodeficiency virus infection; the median age was 38 years. Transmission was suspected to have occurred through sexual activity in 95% of the people infected. While the strain responsible for the current outbreak, clade 1b, is more severe, only a fraction of cases (10%) have been lab-confirmed so far.”
If 95% of cases occurred through sexual activity and in immunodeficiency conditions, there is no need to involve minor children in the “vaccination” campaign. If you are wiser now than you were during Plandemic 1.0 then you should know better than to believe the sources that committed or contributed to worldwide genocide. Make no mistake, Plandemic 2.0 is coming and don’t forget the Bird Flu scam is also waiting in the wings. Resist, refuse, do not submit!
The very reason that Moneypox was selected as the best "candidate" for the next pandemic was that it is largely confined to Africa where "vague and confusing" data is much more easily manipulated. Or created?