WHO's Temporary Recommendations Regarding Mpox
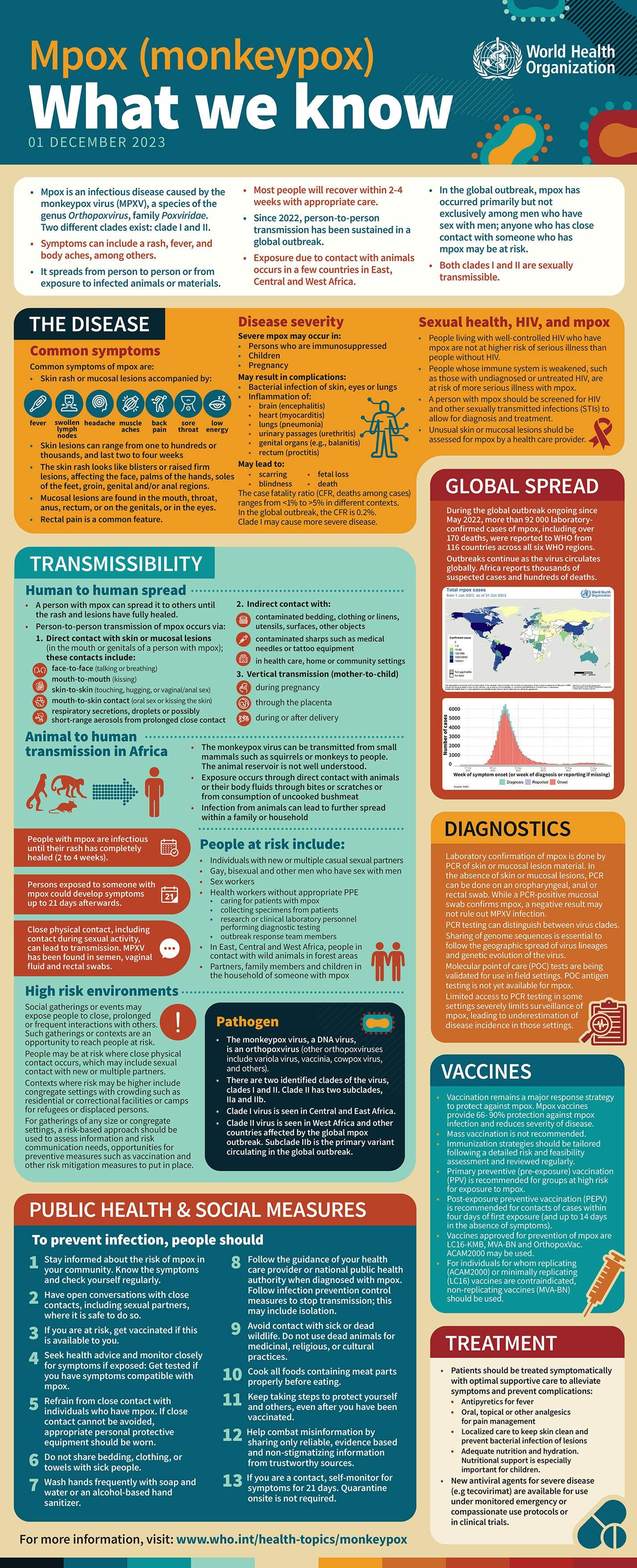
The WHO has published their official temporary recommendations regarding Mpox and they have also renewed the existing standing recommendations for one more year.
Please watch the 6 minute video below…
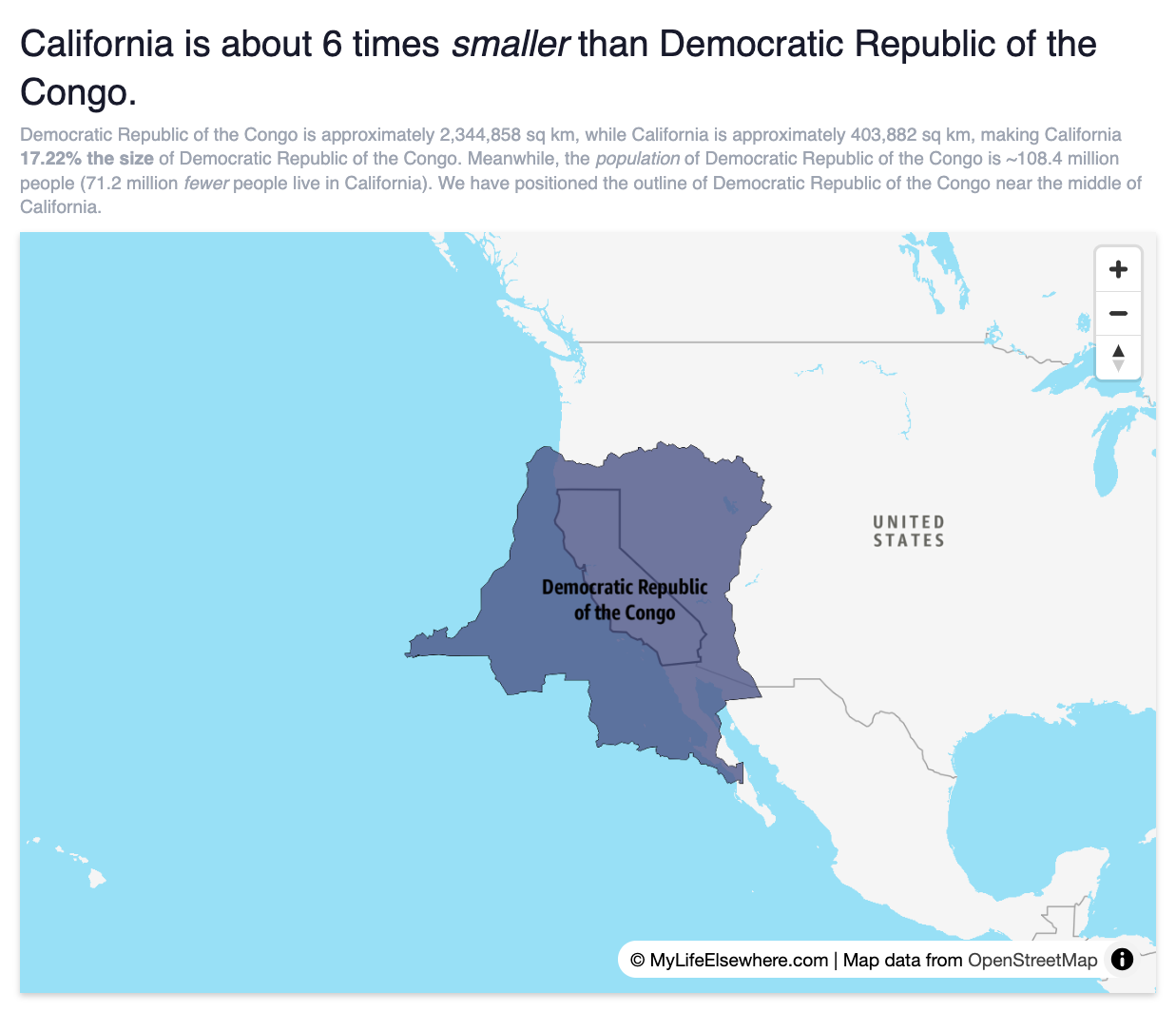
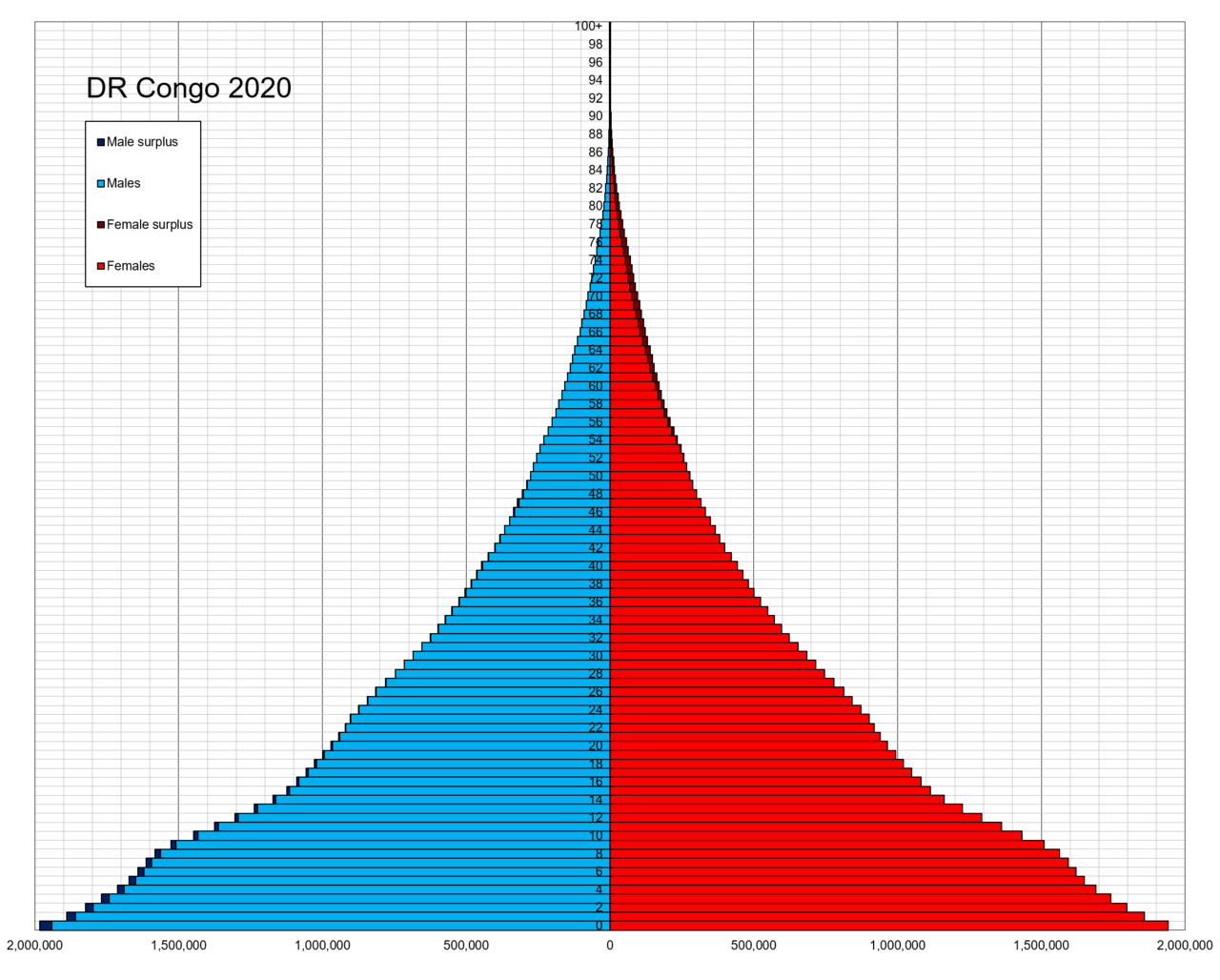
The population of the Democratic Republic of the Congo is over 109 million people.
Temporary Recommendations:
These temporary recommendations are issued to States Parties experiencing the upsurge of mpox, including, but not limited to, the Democratic Republic of the Congo and Burundi, Kenya, Rwanda, and Uganda.
They are intended to be implemented by those States Parties in addition to the current standing recommendations for mpox, which will be extended until 20 August 2025.
In the context of the global efforts to prevent and control the spread of mpox disease outlined in the WHO Strategic framework for enhancing prevention and control of mpox- 2024-2027, the aforementioned standing recommendations apply to all States Parties.
All current WHO interim technical guidance can be accessed on this page of the WHO website. WHO evidence-based guidance has been and will continue to be updated in line with the evolving situation, updated scientific evidence, and WHO risk assessment to support States Parties in the implementation of the WHO Strategic Framework for enhancing mpox prevention and control.
Pursuant to Article 3 Principle of the International Health Regulations (2005) (IHR), the implementation of these temporary recommendations, as well as of the standing recommendations for mpox, by States Parties shall be with full respect for the dignity, human rights and fundamental freedoms of persons, in line with the principles set out in Article 3 of the IHR.
===
Emergency Coordination
Establish or enhance national and local emergency response coordination arrangements;
Establish or enhance the coordination of all partners and stakeholders engaged in or supporting response activities through cooperation, including by introducing accountability mechanisms;
Engage partner organizations for collaboration and support, including humanitarian actors in contexts with insecurity or areas with internal or refugee population displacements and hosting communities insecure areas;
Collaborative Surveillance and Laboratory Diagnostics
Enhance surveillance, by increasing the sensitivity of the approaches adopted and ensuring comprehensive geographical coverage;
Expand access to accurate, affordable and available diagnostics to differentiate monkeypox virus clades, including through strengthening arrangements for the transport of samples, the decentralization of diagnostics, and arrangements to conduct genomic sequencing;
Identify, monitor and support the contacts of people with mpox to prevent onward transmission;
Scale up efforts to thoroughly investigate cases and outbreaks of mpox disease to elucidate the modes of transmission, and prevent its onward transmission to household members and communities;
Report to WHO suspect, probable and confirmed cases of mpox in a timely manner and on a weekly basis;
Safe and Scalable Clinical Care
Provide clinical, nutritional and psychosocial support for patients with mpox, including, as warranted and possible, isolation in care centres and guidance for home-based care;
Develop and implement a plan to expand access to optimised supportive clinical care for all patients with mpox, including children, patients living with HIV and pregnant women. This includes offering HIV tests to adult patients who do not know their HIV status and to children as appropriate, with linkages to HIV treatment and care services when indicated; the prompt identification and effective management of endemic co-infections, such as malaria, varicella zoster and measles viruses, and other sexually transmitted infections (STIs) among cases linked to sexual contact;
Strengthen health and care workers’ capacity, knowledge and skills in the clinical and infection and prevention and control pathways –from diagnosis to discharge of patients with suspected and confirmed mpox –, and provide them with personal protective equipment;
Promote and implement infection prevention and control measures and basic water and sanitation services in health care facilities, household settings, congregate settings (e.g. prisons, internally displaced persons and refugee camps, schools, etc.), and cross border transit areas;
International traffic
Establish or strengthen cross-border collaboration arrangements for surveillance and management of suspect cases of mpox, the provision of information to travellers and conveyance operators, without resorting to general travel and trade restrictions unnecessarily impacting local, regional or national economies;
Vaccination
Prepare for the introduction of mpox vaccine for emergency response through convening of national immunization technical advisory groups, briefing of national regulatory authorities, preparing national policy mechanisms to apply for vaccines through available mechanisms;
Initiate plans to advance mpox vaccination activities in the context of outbreak response in areas with incident cases (i.e. with disease onset in the previous 2-4 weeks), targeting people at high risk of infection (e.g., contacts of cases, including sexual contacts, children, and health and health care workers). This entails the agile adaptation of immunization strategies and plans to concerned areas; the availability of vaccines and supplies; the proactive community engagement, to generate and sustain demand for and trust in vaccination; and the collection of data during vaccination according to implementable research protocols;
Risk communication and community engagement
Strengthen risk communication and community engagement systems with affected communities and local workforces for outbreak prevention, response and vaccination strategies, including through training, mapping high risk and vulnerable populations, social listening and community feedback, managing misinformation. This entails, inter alia, communicating effectively the uncertainties regarding the natural history of mpox, updated information about mpox including information from ongoing clinical trials, about the efficacy of vaccines against mpox, and the uncertainties regarding duration of protection following vaccination;
Address stigma and discrimination of any kind via meaningful community engagement, particularly in health services and during risk communication activities;
Governance and financing
Galvanize and scale up national funding and explore external opportunities for targeted funding of prevention, readiness and response activities;
Integrate mpox prevention and response measures in existing programmes aimed at prevention, control and treatment of other endemic diseases – especially HIV, as well as STIs, malaria, tuberculosis, and COVID-19, as well as non-communicable diseases –, striving, to the extent possible, not to negatively impact their delivery;
Addressing research gaps
Invest in addressing knowledge gaps and in generating evidence, during and after outbreaks, regarding the dynamics of transmission of mpox, risk factors, the social and behavioural drivers of transmission, the natural history of disease, through trials for novel therapeutics and vaccines against mpox, the effectiveness of public health interventions, with a One Health approach;
Reporting on the implementation of temporary recommendations
Report quarterly to WHO on the status of, and challenges related to the implementation of these temporary recommendations, using a standardized tool and channels that will be made available WHO.
SOURCE:
NOTES:
The definition of a confirmed “case” of Mpox is based on the use of the PCR process. Please review the information here: PCRfraud.com
Confirmed case
A person with laboratory confirmed MPXV infection by detection of unique sequences of viral DNA by real-time polymerase chain reaction (PCR)c and/or sequencing.
Probable case
A person presenting with an unexplained acute skin rash, mucosal lesions or lymphadenopathy (swollen lymph nodes). The skin rash may include single or multiple lesions in the ano-genital region or elsewhere on the body. Mucosal lesions may include single or multiple oral, conjunctival, urethral, penile, vaginal, or anorectal lesions. Ano-rectal lesions can also manifest as ano-rectal inflammation (proctitis), pain and/or bleeding.
AND
One or more of the following:
• has an epidemiological link to a probable or confirmed case of mpox in the 21 days before symptom onset
• has had multiple and/or casual sexual partners in the 21 days before symptom onset
• has a positive test result for orthopoxviral infection (e.g., OPXV-specific PCR without MPXV-specific PCR or sequencing)
Suspected case
i) A person who is a contact of a probable or confirmed mpox case in the 21 days before the onset of signs or symptoms, and who presents with any of the following: acute onset of fever (>38.5°C), headache, myalgia (muscle pain/body aches), back pain, profound weakness, or fatigue.
OR
ii) A person presenting with an unexplained acute skin rash, mucosal lesions or lymphadenopathy (swollen lymph nodes). The skin rash may include single or multiple lesions in the ano-genital region or elsewhere on the body. Mucosal lesions may include single or multiple oral, conjunctival, urethral, penile, vaginal, or anorectal lesions. Ano-rectal lesions can also manifest as ano-rectal inflammation (proctitis), pain and/or bleeding.
AND
for which the following common causes of acute rash or skin lesions do not fully explain the clinical picture: varicella zoster, herpes zoster, measles, herpes simplex, bacterial skin infections, disseminated gonococcus infection, primary or secondary syphilis, chancroid, lymphogranuloma venereum, granuloma inguinale, molluscum contagiosum, allergic reaction (e.g., to plants); and any other locally relevant common causes of papular or vesicular rash.
N.B. It is not necessary to obtain negative laboratory results for listed common causes of rash illness in order to classify a case as suspected. Further, if suspicion of mpox or MPXV infection is high due to either history and/or clinical presentation or possible exposure to a case, the identification of an alternate pathogen which causes rash illness should not preclude testing for MPXV, as co-infections have been identified.
Public Health Advice on protecting yourself and others from mpox
Public Health Advice for men who have sex with men on preventing mpox
Public Health Advice for gatherings during the mpox outbreak
Public Health Advice for gay, bisexual and other men who have sex with men on mpox
Public Health Advice on mpox and sex-on-premises venues and events
SOURCE:
https://www.who.int/emergencies/outbreak-toolkit/disease-outbreak-toolboxes/mpox-outbreak-toolbox
James Roguski
310-619-3055
JamesRoguski.substack.com/archive
All content is free to all readers.
All support is deeply appreciated.








I’m not participating, just like I didn’t participate in the Covid bs.
wow, so there is a war in Goma, and camps of people in horrid conditions. hummm, did I understand that correctly. malnourished abusive conditions. and they want a money jab to take care of the problem.
it's really time to talk health conditions of people. get to root cause of symptoms. many of us are just not buying it anymore. and demand better humantarian ethical responses
and here we go again with contact tracing, fake testing, and isolation. insanity 2.0