PCR "Test" Injuries
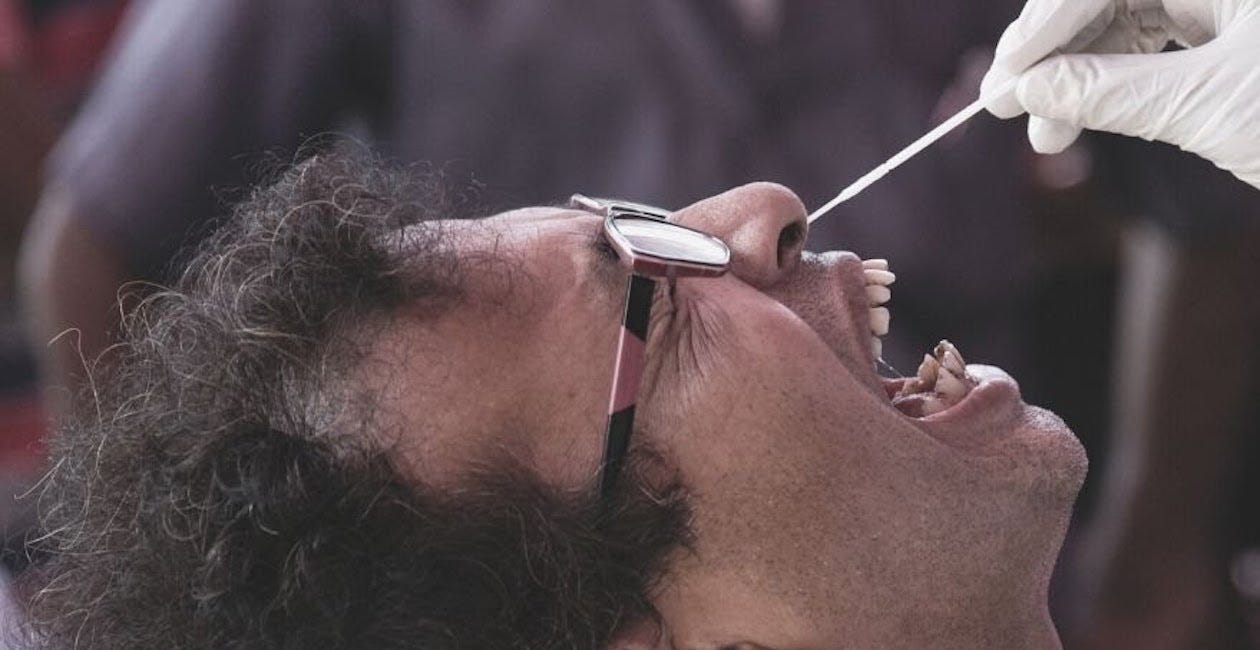
The fraudulent PCR "test" is a medical procedure that is often done improperly, resulting in devastating and permanent injury. PLEASE REMEMBER THAT YOU ALWAYS HAVE THE RIGHT TO SAY NO.
At least two children have DIED due to injuries caused by PCR “tests” for COVID-19.
Angela Tondi was injured by the swab used to perform the PCR "test." The swab was inserted into her nose in a painful manner and caused her to start leaking CerebroSpinal Fluid (CSF). It resulted in severe headaches, meningitis and it has affected her sense of smell and taste to the point that she was barely able to eat.
Please watch the video below:
https://rumble.com/v5abef9-pcr-injury.html
The source video for the excerpt above is located HERE.
Your unalienable right of INFORMED DISSENT requires that you be properly informed before giving your consent to ANY medical procedure.
Poorly trained personnel have conducted this procedure improperly on untold millions of people.
Practically no one was ever properly and fully informed regarding the potential for harm by this fraudulent medical “test.”
YOU ALWAYS HAVE THE RIGHT TO SAY NO.
Realize that every medical procedure comes with risks.
It is your health care practitioner’s responsibility to explain those risks to you before beginning any procedure.
Please review the published articles below.
June 11, 2020
Adverse effects of nasopharyngeal swabs: Three-dimensional printed versus commercial swabs
Epistaxis [NOSEBLEED] occurred immediately or shortly following the removal of the swab in 5.0% of employees tested with the 3D swab and in 8.3% of employees tested with the commercial swab.
Epistaxis was usually mild and self-limited, although 1 employee required an emergency department visit for ongoing epistaxis after testing with a commercial swab. Other minor adverse effects included nasal discomfort, headache, earache, and rhinorrhea, which typically lasted hours to a day.
JULY 15, 2020
Child dies after COVID-19 test in Saudi Arabia
Abdulaziz, an 18-month Saudi toddler, died last week when a swab broke inside his nose while doctors were determining whether he suffered from COVID-19 virus.
The boy had a fever and was taken to Shaqra General Hospital in central Saudi Arabia by his parents. Medical staff tested the boy because they suspected his high temperature might be due to COVID-19.
During the test, the swab broke inside the child’s nose.Doctors performed an operation to extract the swab, which they said was successful, the child’s uncle was quoted by local media as saying.
When the child woke up following the surgery, his mother repeatedly asked medical staff to check up on her son but a doctor never arrived. At 9 a.m. the child fainted and lost consciousness.
The uncle said x-rays showed a blockage in the child’s airway. As his condition was deteriorated, his uncle demanded he be transferred to a specialist hospital in Riyadh but the child died even before the arrival of an ambulance.
“I am awaiting the punishment of the person responsible for the child’s death and society must be protected from such practices,” said the child’s uncle.
The child’s father, Abdullah Bin Abdulaziz Al-Jawfan, received a call from the Saudi Health Minister, Tawfiq Al-Rabiah, in which he expressed his condolences and pledged to follow up on the child's case himself. Shaqra is a small city located about 190 km north-west of the capital Riyadh.
July 28, 2020
Test, test, test – a complication of testing for coronavirus disease 2019 with nasal swabs
Case report
A male nursing home resident in his late seventies presented to the emergency department after an unwitnessed fall, unable to mobilise. He had a background of severe dementia and chronic kidney disease. He was diagnosed with a right-sided neck of femur fracture. He was admitted and underwent an uncomplicated right-sided hemi-arthroplasty.
Three days post-operatively, he developed a low grade fever. He was suspected of having Covid-19 as he had been in contact with other patients on the ward who had subsequently tested positive for the virus.
The patient lacked capacity and was uncooperative whilst undergoing a nasopharyngeal swab test for Covid-19. Despite gentle restraint from a trained healthcare assistant, rapid head movements resulted in the engagement of the swab breakpoint mechanism, whilst the swab was still in the nasal cavity. The swab was retained in the nose out of direct vision.
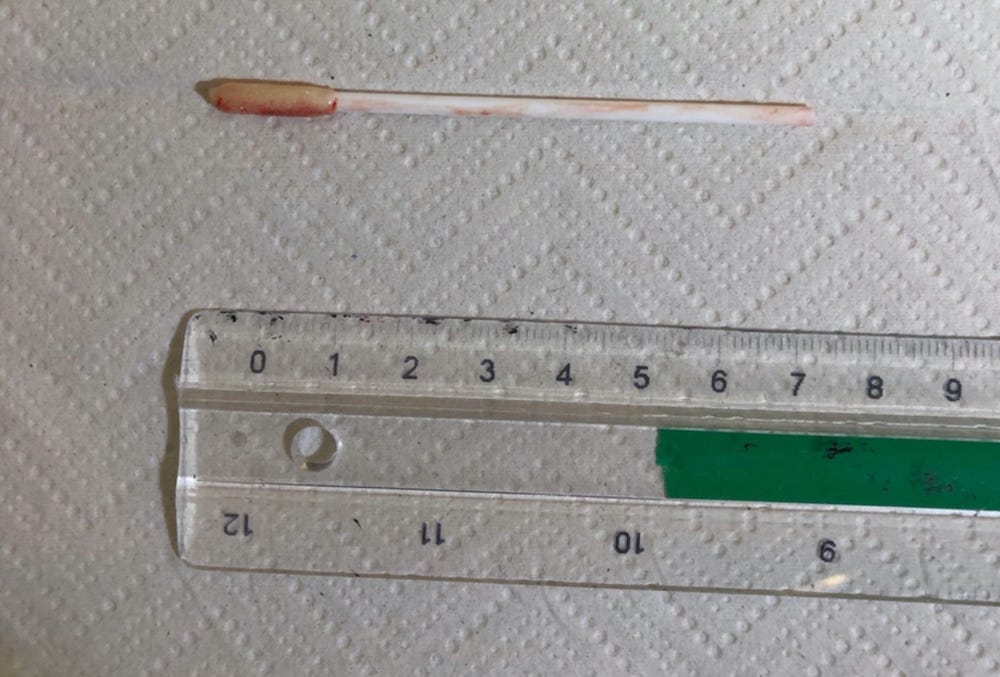
The ENT registrar was called to retrieve the swab. The patient underwent a bedside examination with a flexible nasendoscope. A nasal swab stick was found in the right nasal cavity, under the inferior turbinate on the floor, midway in the nasal cavity (Figure 1). Retrieval of an 8 cm swab was performed with minimal trauma under direct vision using Tilley's dressing forceps.
August 28, 2020
Tripura woman whose newborn died after swab collection files complaint
The woman in her complaint said her baby was healthy till the collection of his swab samples after which he started bleeding from the nose and died shortly thereafter.
Almost two weeks following the death of a three-day old baby who died shortly after his swab samples were taken for Covid-19 test, the baby’s mother filed a complaint with the police against doctors at the hospital and accused them of negligence.
Police said that the woman lodged the complaint on Thursday from the baby’s mother and they have already started an investigation.
“The incident happened earlier this month. We have started investigation under Section 157 CrPc,” said Subimal Barman, officer in-charge of New Capital Complex police station.
He added that the woman had been admitted to the hospital as she had tested positive for Covid-19 positive. She lodged the complaint after she was released from the hospital recently.
The baby was born at the state-run Govind Ballabh Panth (GBP) hospital on August 10 and he died on August 12. Samples of the baby were taken as his mother was then Covid-19 positive. The woman was recently released from the hospital after she was tested negative.
A day after the baby’s death, the state government constituted a three-member team for a departmental inquiry into death of the baby.
“The committee submitted its report based on its inquiry to the state government recently. The report is with the government,” said director of Directorate of Health Services Dr. Subhasish Debbarma.
September 17, 2020
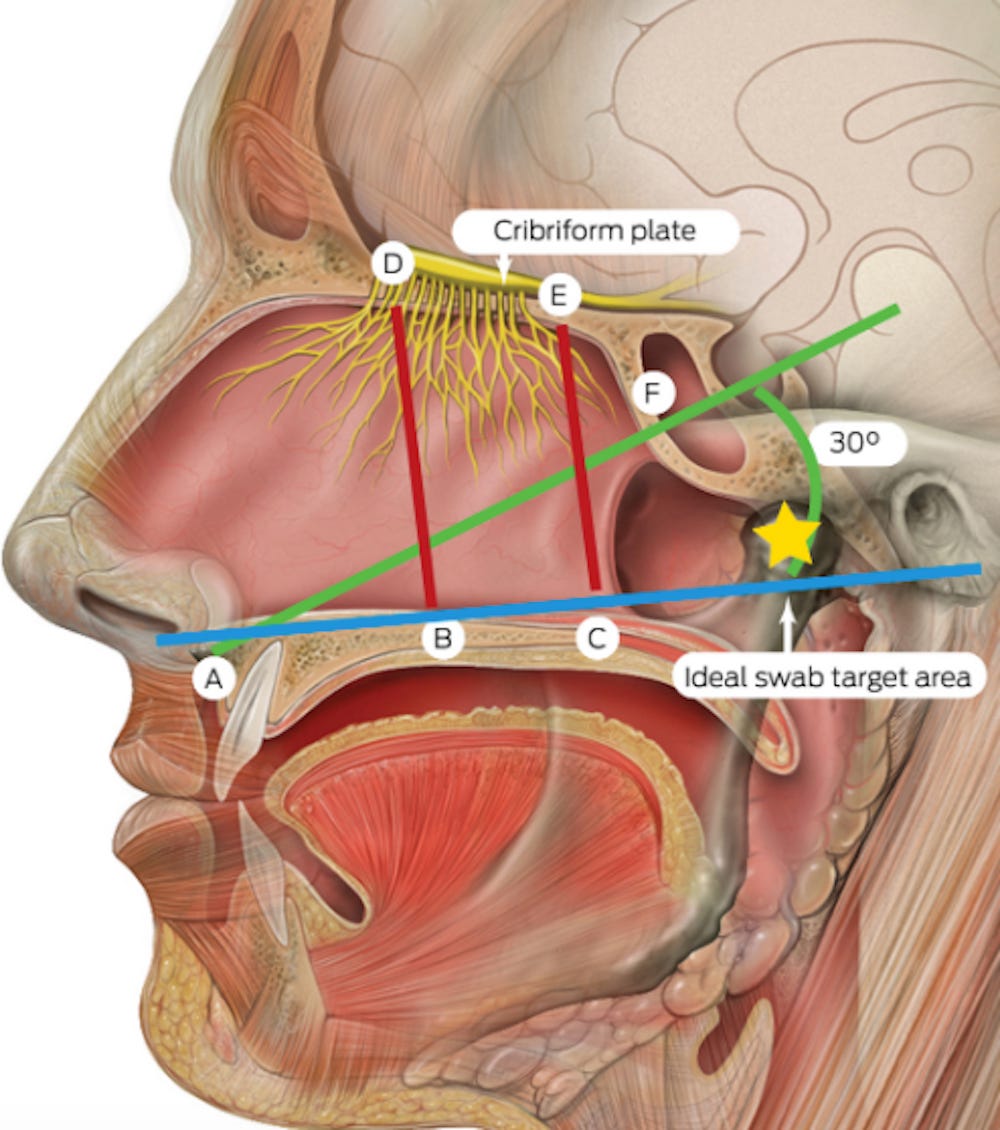
SARS-CoV-2 Nasopharyngeal Swab Testing—False-Negative Results From a Pervasive Anatomical Misconception
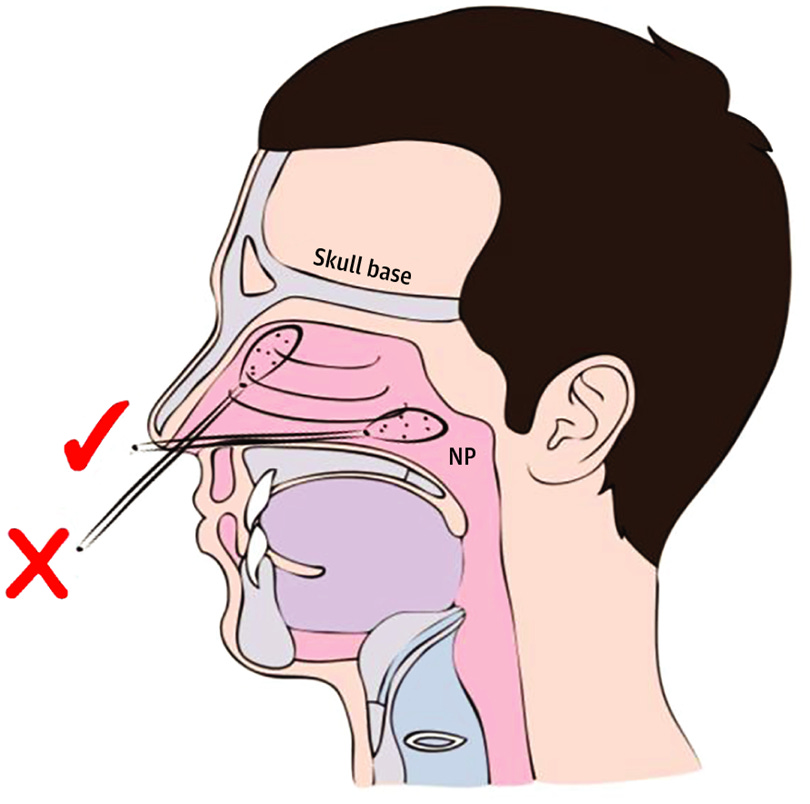
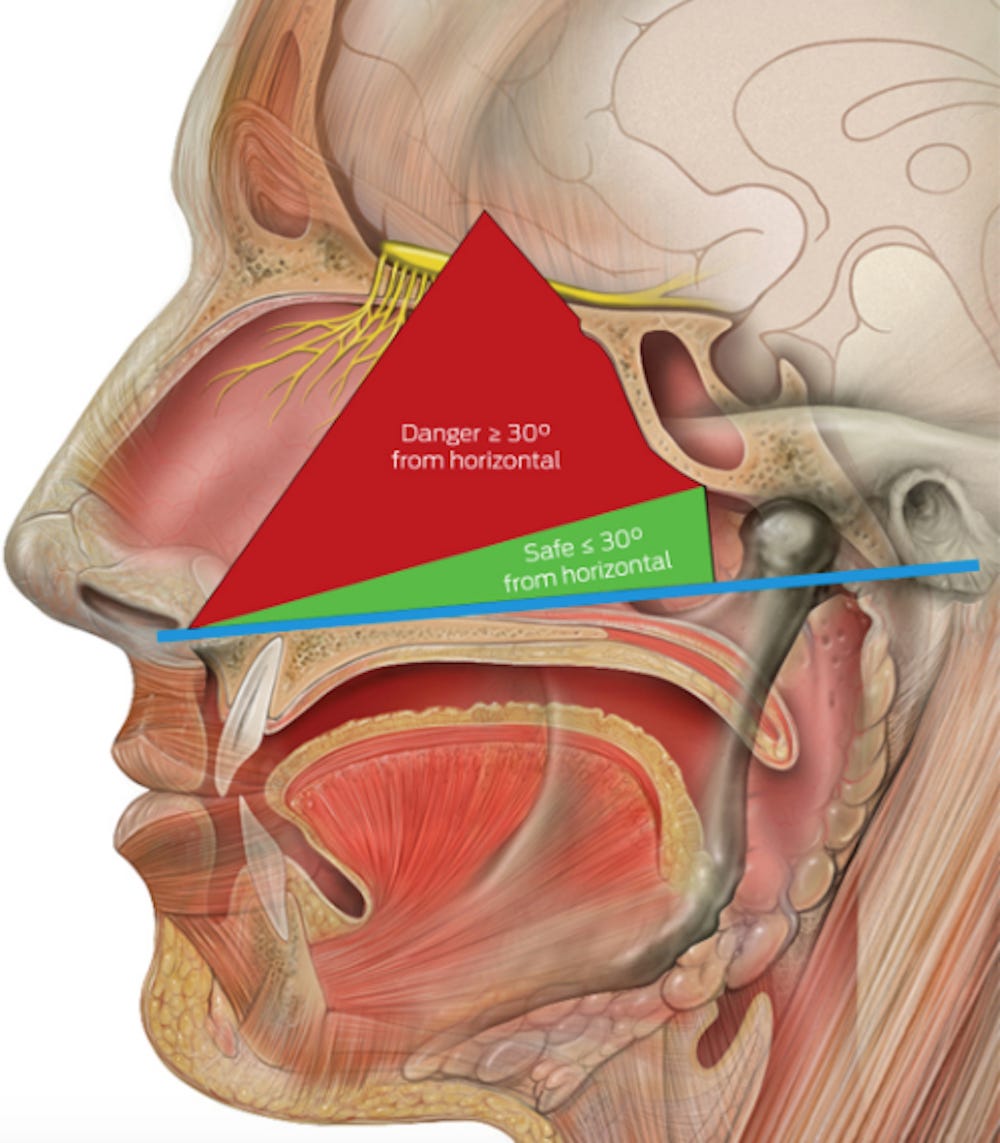
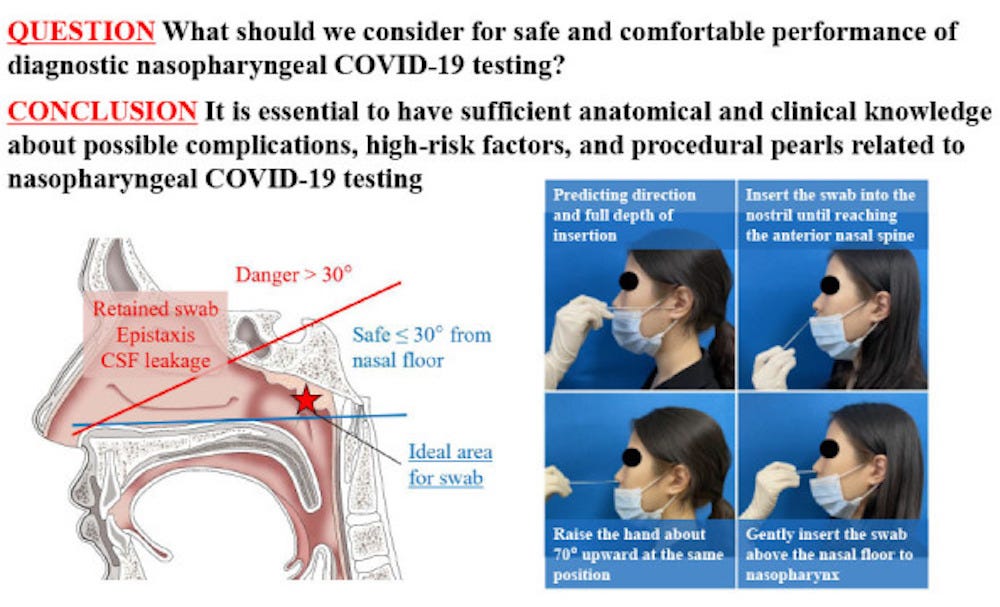
The trajectory from the nostril to the nasopharynx is often presumed to be along the dorsum of the nose, likely because of the visual appearance of the external nose. In reality, the correct trajectory is along the floor of the nose in the direction back toward the ear.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2770786
September 20, 2020
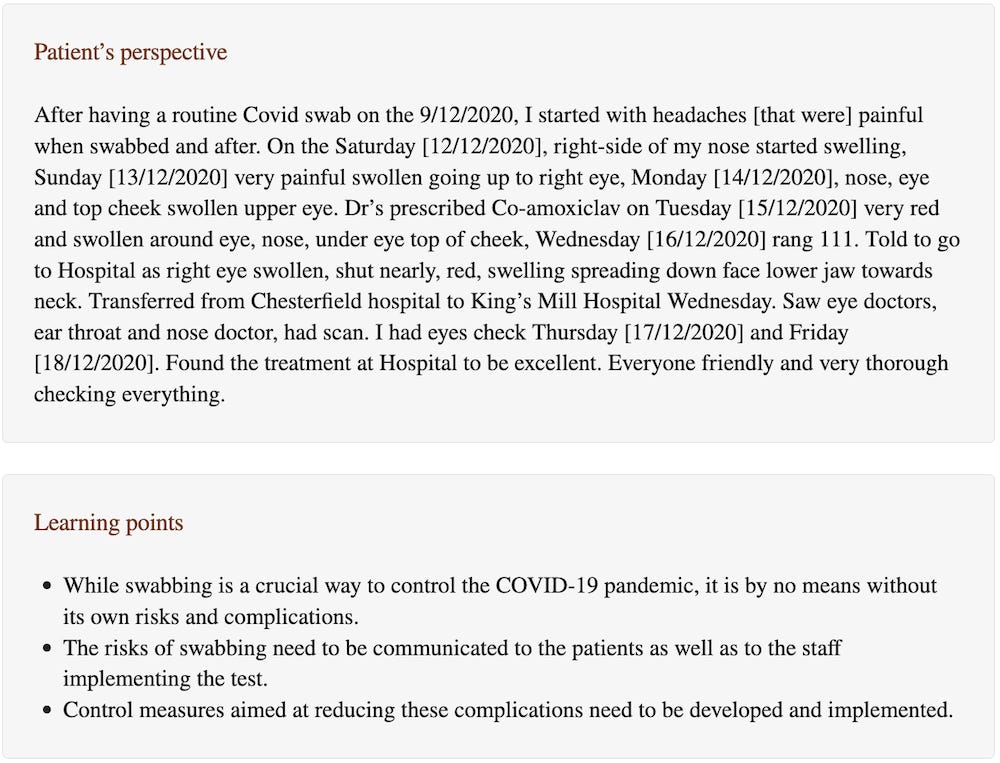
Is naso-pharyngeal swab always safe for SARS-CoV-2 testing? An unusual, accidental foreign body swallowing
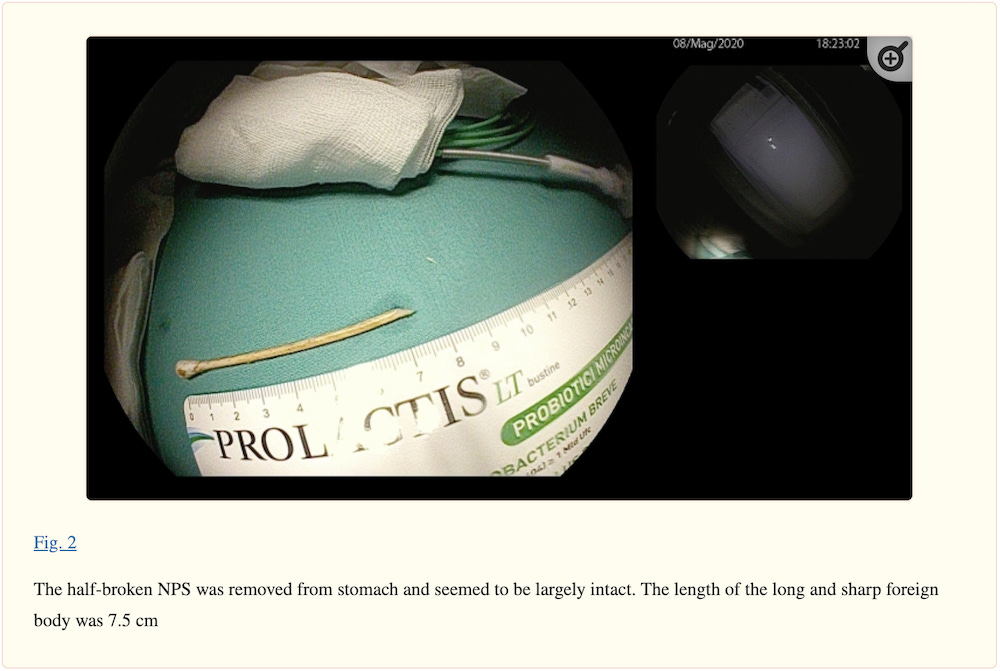
We present a case of a 47-year-old male with no known comorbidity, who accidentally swallowed a portion of a naso-pharyngeal swab half-broken during the second diagnostic test for SARS-CoV-2. The intact swab had a total length of 15 cm and was made of wood.
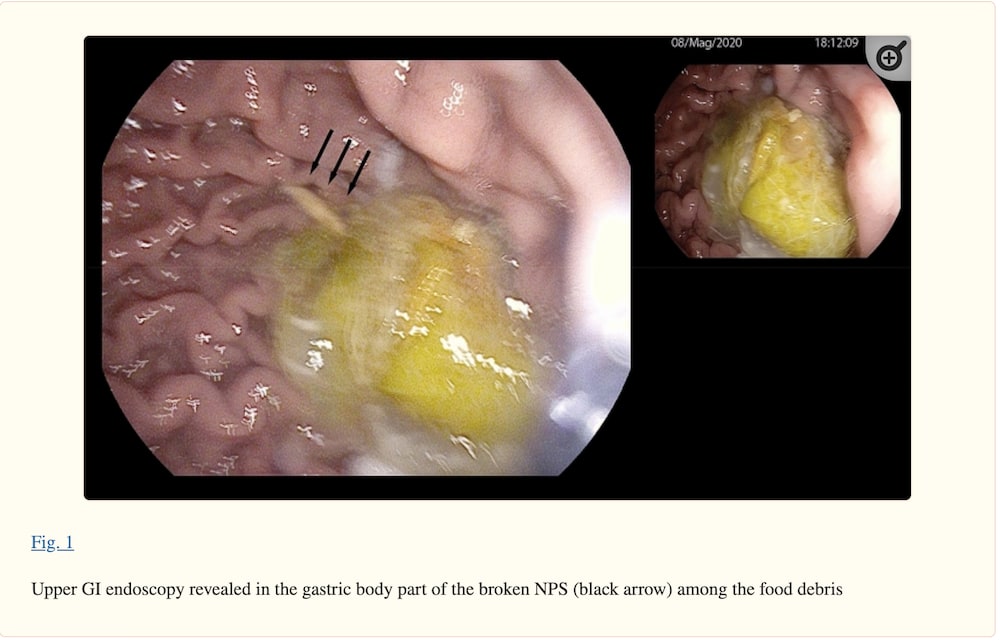
Upper gastrointestinal endoscopy was promptly performed to prevent the long sharp swab from crossing the pylorus leading to serious complications and, therefore, risk surgical intervention. The patient was intubated and the procedure was carried out under general anesthesia. In the gastric body, broken naso-pharyngeal swab was detected among the food debris, and using a latex rubber hood, the 7.5 cm foreign body was removed with a retrieval alligator-tooth forceps.
October 1, 2020
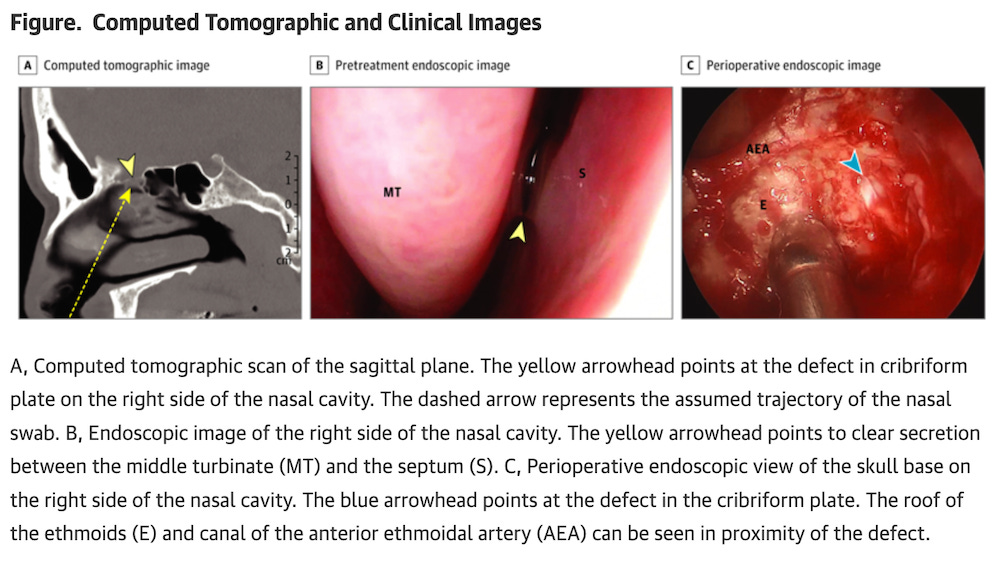
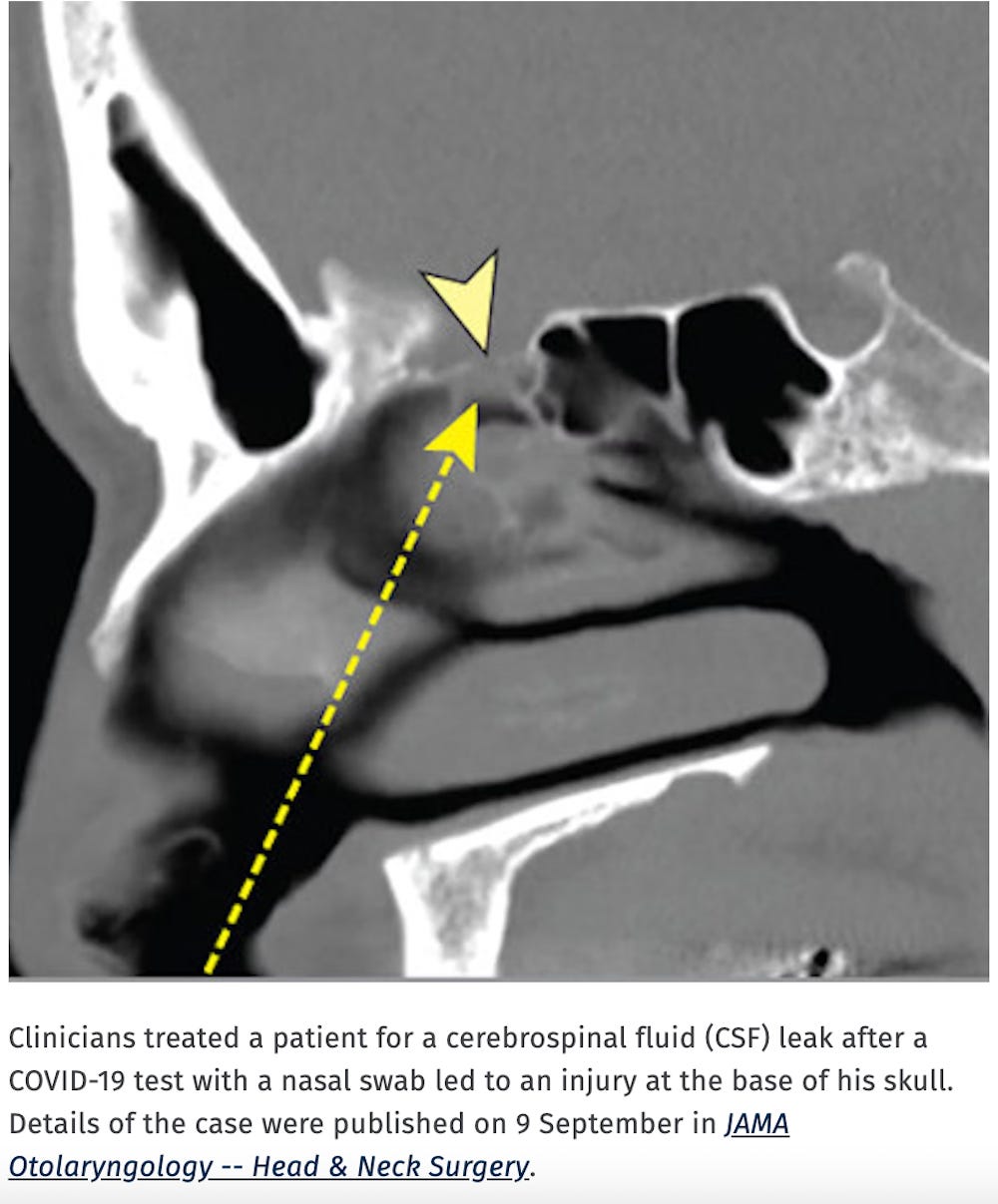
Cerebrospinal Fluid Leak After Nasal Swab Testing for Coronavirus Disease 2019
Encephalocele is a neural tube defect characterized by sac-like protrusions of the brain and the membranes that cover it through openings in the skull.
To our knowledge, this is the first report of an iatrogenic [CerebroSpinal Fluid] CSF leak after a nasal swab for COVID-19.
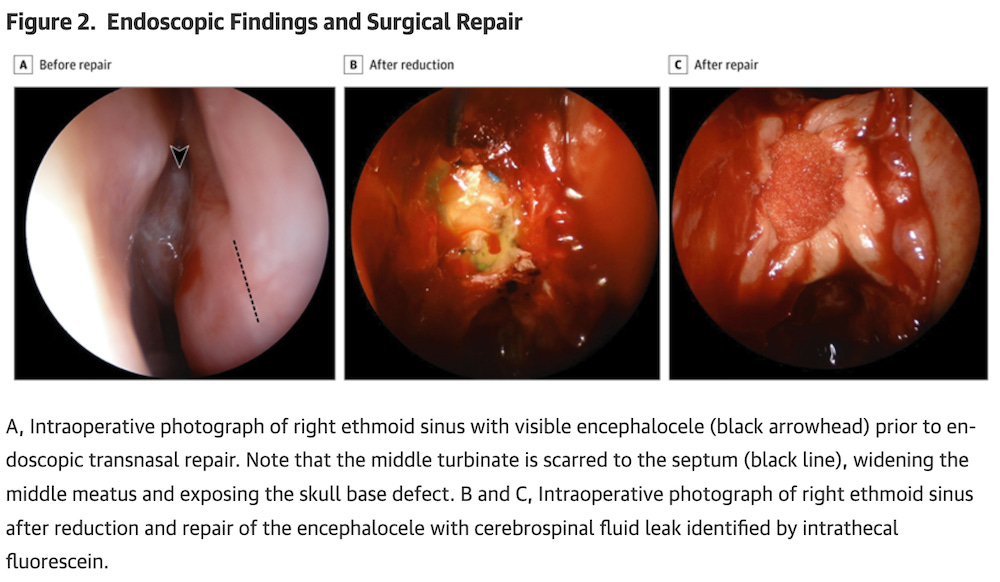
A woman in her 40s presented with unilateral rhinorrhea, metallic taste, headache, neck stiffness, and photophobia. The patient had recently completed nasal COVID-19 testing for an elective hernia repair. Shortly after, she developed unilateral rhinorrhea, headache, and vomiting. The patient’s medical history was notable for idiopathic intracranial hypertension and removal of nasal polyps over 20 years before presentation. Physical examination revealed clear rhinorrhea from the right side. Flexible nasopharyngoscopy revealed a mass in the right anterior middle meatus, but did not identify the source of the fluid. The nasal drainage tested positive for β2-transferrin.
The patient was admitted to the hospital for endoscopic surgical repair. An encephalocele was identified in the right anterior ethmoid cavity. After reduction of the encephalocele, a skull base defect in the fovea ethmoidalis was repaired with a combination of acellular human dermal matrix and a poly(D,L-lactic) acid.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2771362
October 13, 2020
Is oro/nasopharyngeal swab for SARS-CoV-2 detection a safe procedure? Complications observed among a case series of 4876 consecutive swabs
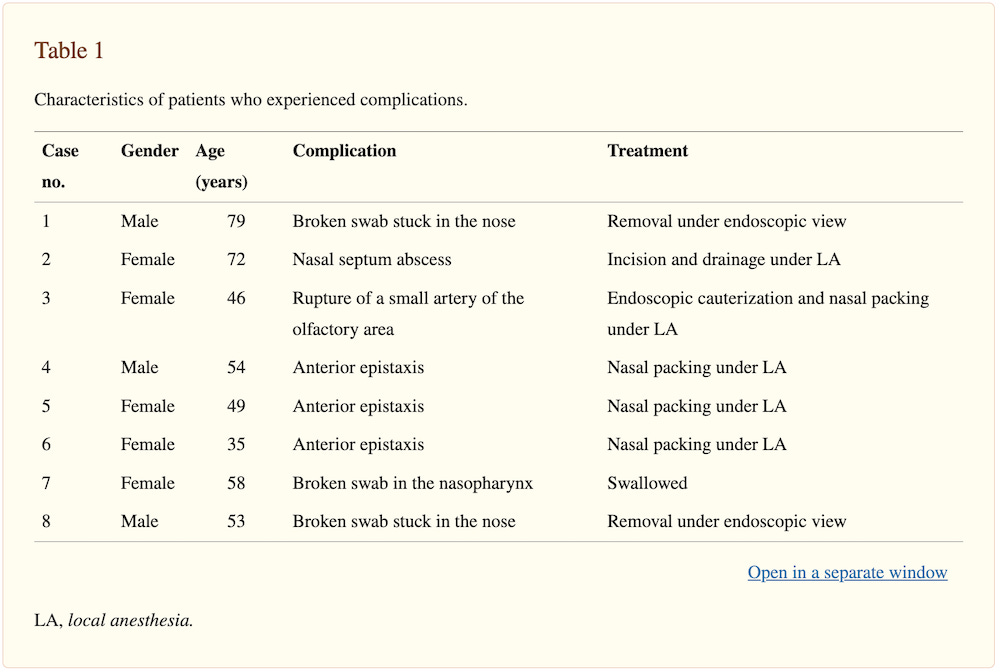
A retrospective review was carried out in June 2020 on 4876 consecutive swabs performed at Treviso Hospital during May 2020 for the detection of SARS-CoV-2. All reports, possible complications and clinical information were noted from registries of the infectious disease units and medical records. Here, we report complications requiring ENT [Ear, Nose and Throat] evaluation.
2 males and 6 females (0.16%), aging from 35 to 79 years (mean age 53.8 yr) required ENT evaluation for complications. Three patients experienced moderate anterior epistaxis [nosebleed] requiring nasal packing.
A further three patients suffered broken and impacted swabs in the nasal cavity, necessitating removal by an otolaryngologist in two cases.
One patient, affected by diabetes mellitus and neutropenia, developed septal abscess (case 2) and another, who later was observed to have septal deviation, had severe anterior and posterior bleeding from an arterial point of the olfactory area, possibly arising from the anterior ethmoidal artery (case 3) requiring surgical cauterization.
February 12, 2021
Meningitis due to cerebrospinal fluid leak after nasal swab testing for COVID‐19
The patient had completed a nasal reverse transcription polymerase chain reaction (RT‐PCR) COVID‐19 testing in March 2020 which came back negative. One week after, she developed unilateral continuous rhinorrhoea with metallic taste. She was then diagnosed of allergic rhinitis by her general practitioner, who prescribed antihistaminics and a short‐term antibiotherapy (amoxicillin‐clavulanic), with no resolution of the symptoms. In July 2020, a nasal drainage tested positive for β2‐transferrin and head computed tomography was performed identifying a CSF fistula at the lamina cribrosa.
February 20, 2021
CSF Leak After COVID‐19 Nasopharyngeal Swab: A Case Report
Encephalocele is a neural tube defect characterized by sac-like protrusions of the brain and the membranes that cover it through openings in the skull.
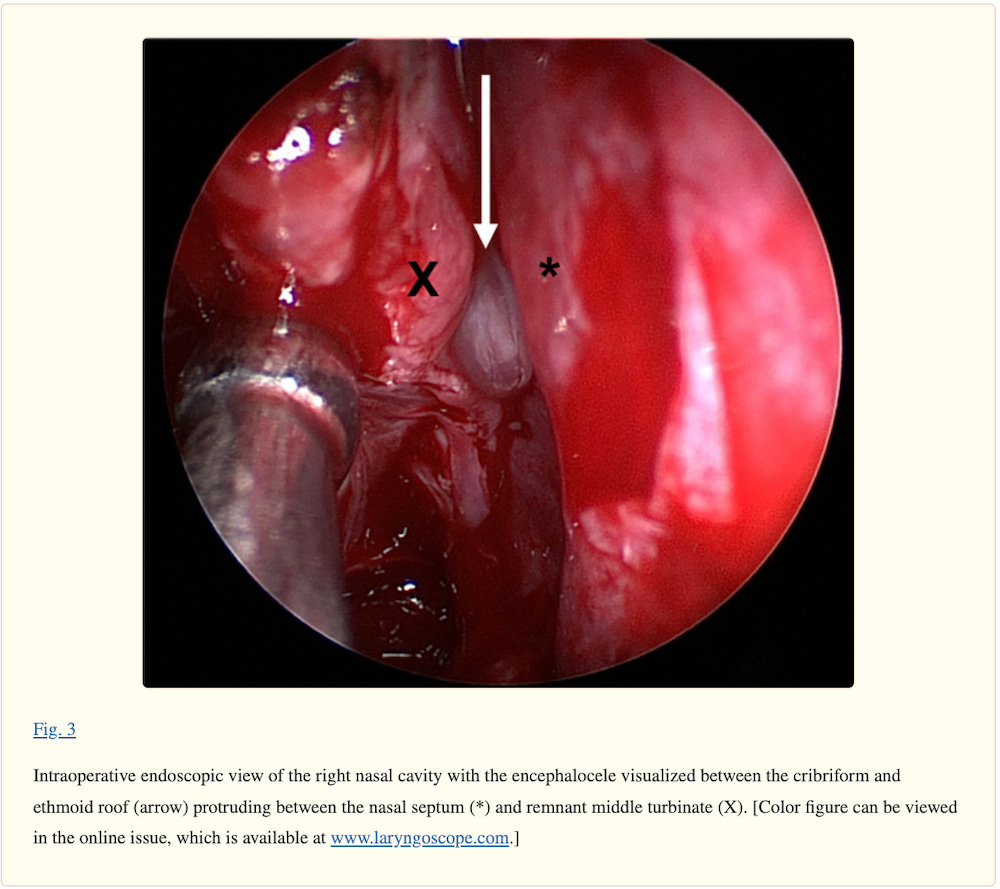
The patient is a 38‐year‐old female who presented to our hospital after experiencing severe pain during an [nasopharyngeal] NP swab for COVID followed by 2 days of persistent clear watery rhinorrhea that worsened with leaning forward. She also noticed persistent headache and metallic tasting postnasal drip. The patient had no history of head trauma or surgery. She was otherwise healthy.
Initial exam, including nasal endoscopy, was unremarkable other than a small amount of clear right‐sided nasal drainage. The patient underwent a computed tomography scan, which demonstrated a subtle defect in the posterior right cribriform plate. She then underwent magnetic resonance imaging, which demonstrated a small encephalocele projecting from the olfactory fossa of the right superior nasal cavity.
February 26, 2021
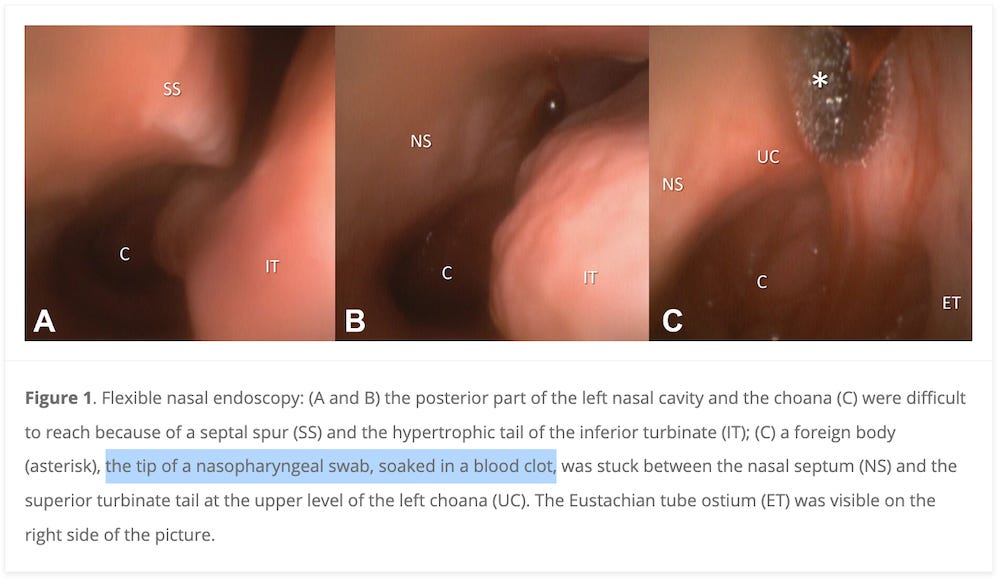
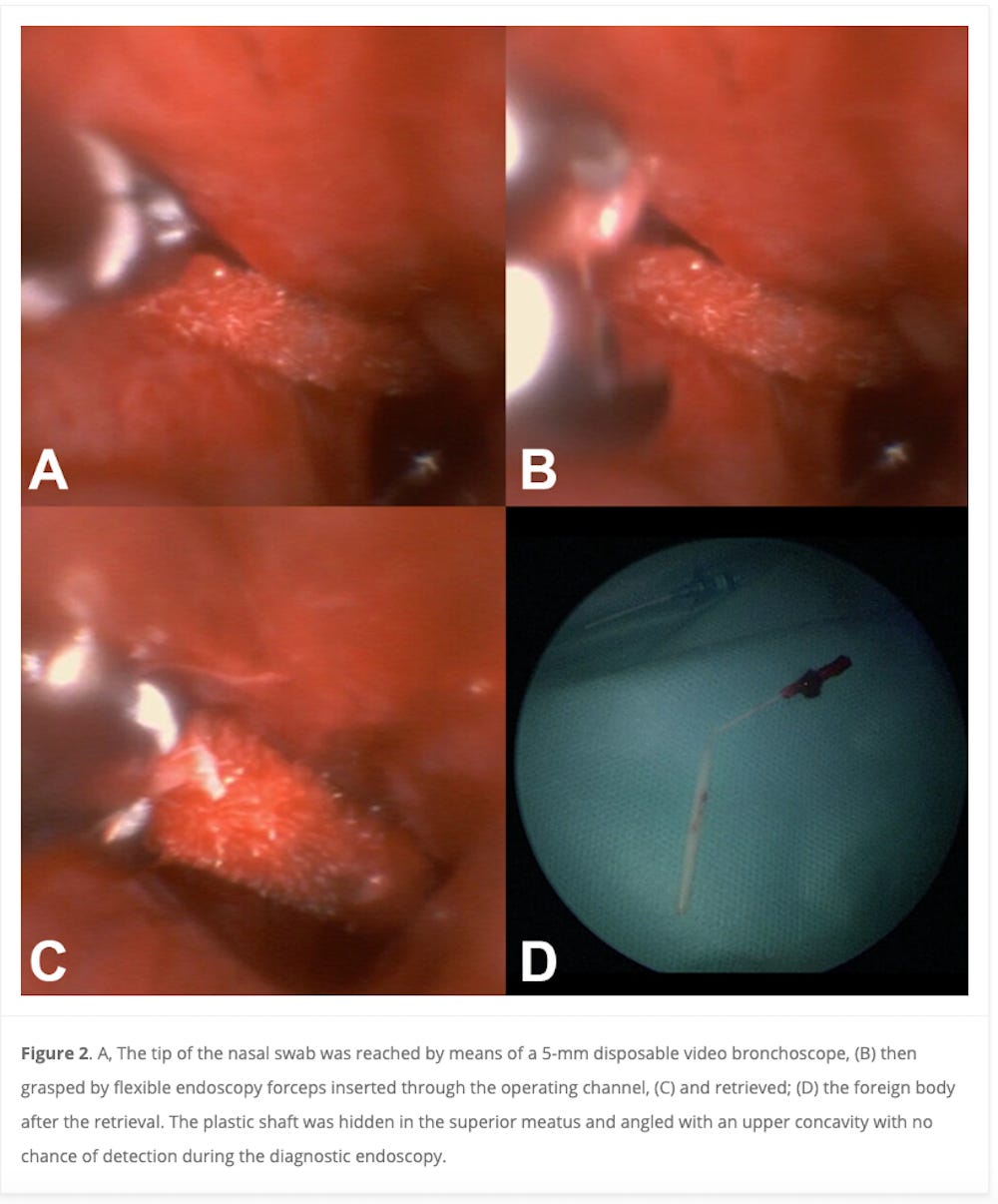
An Unusual Retained Choanal Foreign Body: A Possible Complication of COVID-19 Testing With Nasopharyngeal Swab
We here describe a complication occurred during NPS collection performed in an uncooperative patient where the plastic shaft of the swab fractured during the testing procedure, resulting in swab tip retention deep into the nasal cavity.
A 37-year-old noncompliant male with Down syndrome presented to the emergency department (ED) after an attempt of COVID-19 testing at his day care facility performed because of a close contact with a confirmed case. During the procedure, a sudden head movement led to the engagement of swab tip break point mechanism while the NPS was still in the left nasal cavity resulting in swab tip retention deep into the nasal cavity, completely out of direct vision.
Informed consent for patient information and images to be published was provided by the legally authorized patient’s representative.
In our case, the shaft of the swab consisted of 2 components: a plastic swab, which incorporates a break point halfway down the shaft of the swab, and an open-celled foam tip to collect the specimen. The break point mechanism prevents contamination while transferring the shaft into the container. However, this feature makes the swab susceptible to fracture while still in the nasal cavity.
February 26, 2021
March 4, 2021
Assessment of Available Online Information About Nasopharyngeal Swab Testing in Patient Instructions for Sinus and Pituitary Surgery
The absence of online information regarding risks of SARS-CoV-2 testing for patients with sinus and/or pituitary surgery illustrates an opportunity for patient education that could maximize safety during the pandemic.
Two areas for improvement include
(1) improving clinician knowledge and patient education, and
(2) improving prescreening for SARS-CoV-2 NPS testing.
Clinicians can improve patient education by speaking with high-risk patients and updating their websites/handouts to educate patients about potential injury related to SARS-CoV-2 NPS testing.
Before ordering or performing SARS-CoV-2 testing, health care professionals must identify the population at risk of NPS-related injury.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2777089
Beware of COVID-19 Swab Testing in Those With Past Sinus/Skull Base Surgery
Online information about COVID-19 nasopharyngeal swabs doesn’t warn those with prior extensive sinus or skull base surgery against having the testing.
"Not one site of the 200 we searched online had information cautioning against blind nasopharyngeal swab testing in those with a history of sinus or skull base surgery," said senior author Philip G. Chen, MD, of The University of Texas Health Science Center at San Antonio.
Chen suggests the problem is exacerbated when swabbing is performed incorrectly, noting that, if the swab angle is too high, a puncture can occur.
“Patients at risk of injury from SARS-CoV-2 testing must be educated about potentially adverse testing outcomes.”
April 20, 2021
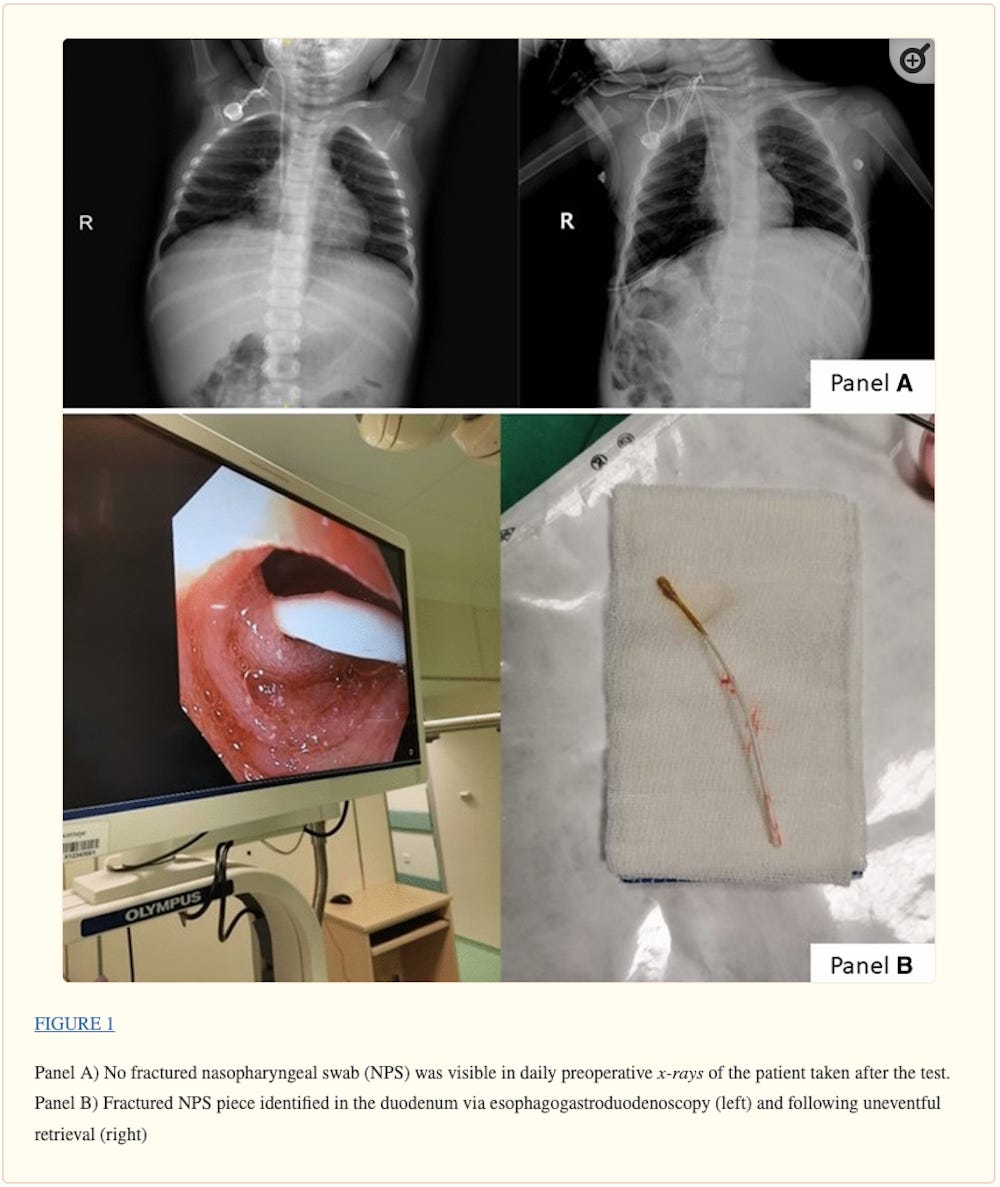
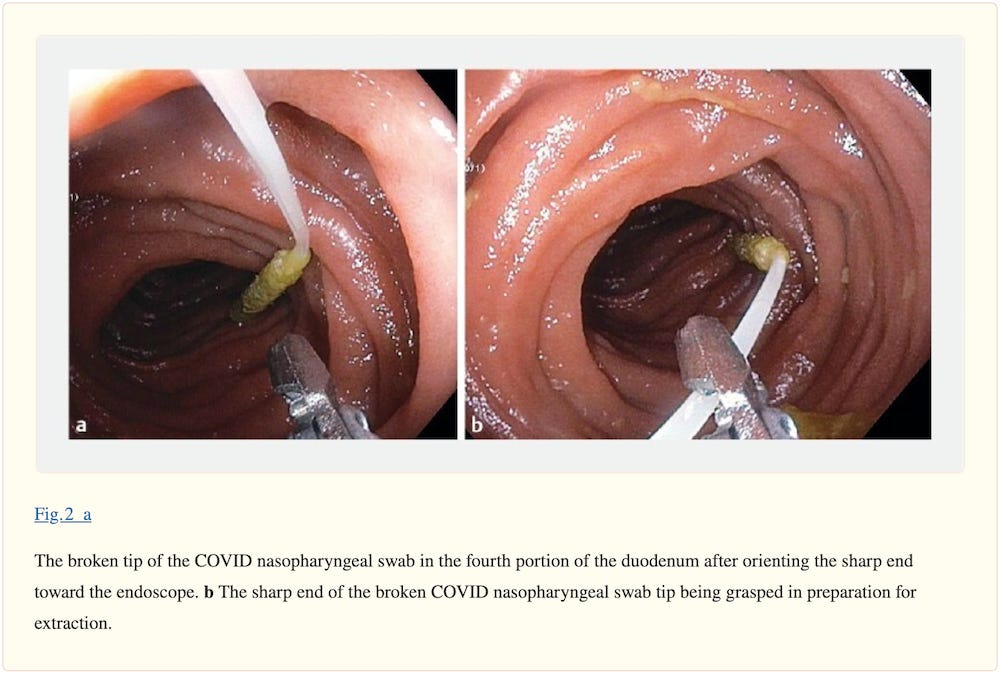
A fractured nasopharyngeal swab in the duodenum of a toddler: an unusual complication of preoperative COVID-19 testing
A 22-month-old female patient was scheduled for neuroblastoma excision. According to our hospital policy, a COVID-19 swab test was performed preoperatively. During the test, the [NasoPharyngeal Swab] NPS fractured because the patient moved suddenly, resulting in the lodgement of approximately 5 cm of the swab stick in the nasopharynx.
The piece could not be visualized with plain sight or on x-ray, and there was no clinical deterioration related to aspiration into the upper airways, for which there was no evidence on chest x-ray. Since the patient exhibited no signs of intestinal obstruction and her surgical intervention was scheduled to be performed within a few days, an exploratory upper gastrointestinal tract endoscopy was planned for the same session.
An esophagogastroduodenoscopy procedure was performed after anesthetic induction followed by endotracheal intubation with an uncuffed tube (internal diameter, 4.5 mm). The NPS fragment was identified in the duodenum and gently retrieved with alligator endoscopic forceps. There was no mucosal injury. The scheduled surgical procedure was performed subsequently; after approximately six hours of surgery, the patient was extubated and transferred to the intensive care unit.
April 28, 2021
COVID‐19 nasopharyngeal swab causing a traumatic cerebrospinal fluid leak
Informed consent [??] was obtained from the patient discussed. A 34‐year‐old lady with 2 days of malaise in conjunction with upper respiratory tract symptoms underwent a nasopharyngeal COVID‐19 swab.
She had no known history of a skull base defect, previous nasal surgery or idiopathic intracranial hypertension. The swab was performed at a drive‐through clinic where the patient remained in her car whilst undergoing the swab.
She experienced a significant amount of pain during the swab with epistaxis immediately following the procedure. Forty‐eight hours following the swab, she developed intermittent clear rhinorrhoea from the right nostril that was precipitated by bending forwards or straining.
Several days later, she presented to an emergency department where she was discharged without testing for beta‐2‐transferrin. She then presented to our institution's emergency department 5 days after the development of rhinorrhoea (7 days after the swab). She was neurologically intact with no features of meningism. A sample at this time was found to be positive for beta‐2‐transferrin, confirming [CerebroSpinal Fluid] CSF rhinorrhoea.
April 29, 2021
Complications of COVID-19 Nasopharyngeal Swab Test
The frequency of complications requiring treatment in the [Emergency Department] ED was 1.24 per 100 000 performed SARS-CoV-2 tests.
The broken swabs were removed via nasal endoscopy under local anesthesia, whereas the nasal bleeds required medication, numerous nasal packings, and surgical and endovascular procedures and led to fetal risk, sepsis, and blood transfusions.
Half of the bleeds were potentially life threatening (hemoglobin level fell below 6.5 g/dL [to convert to g/L, multiply by 10.0]).
Massive bleeding complicated localization of the bleeds.
Infections, as well as intranasal adhesions and septal perforations, likely resulted from the repetitive nasal packings.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2779393
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8085764/
May 18, 2021
COVID-19 swab-related skull base injury
The patient precisely recalled the onset of unilateral clear rhinorrhoea, which occurred within hours of an “extremely painful” coronavirus disease 2019 (COVID-19) swab test.
Given the historical description, time frame and clinical findings, we believe the injury to be a complication of the COVID-19 swab.
May 19, 2021
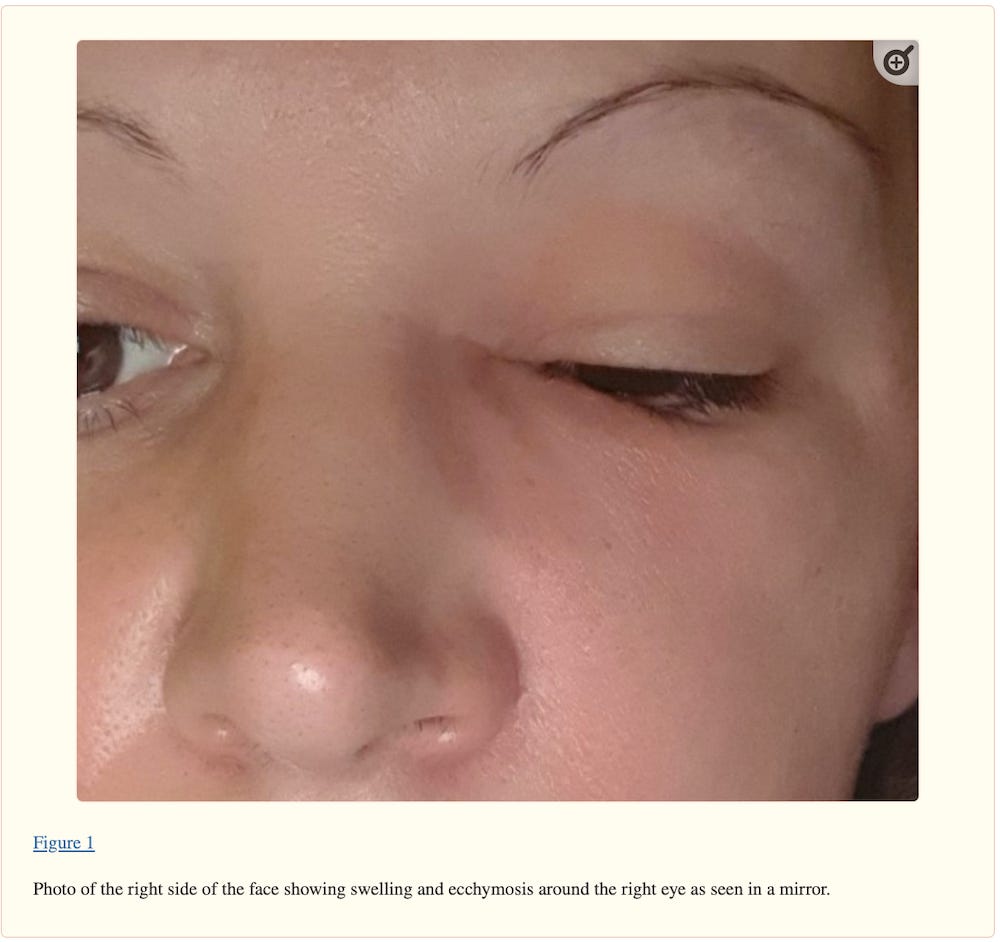
Preseptal cellulitis and infraorbital abscess as a complication of a routine COVID-19 swab
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8137238/
May 28, 2021
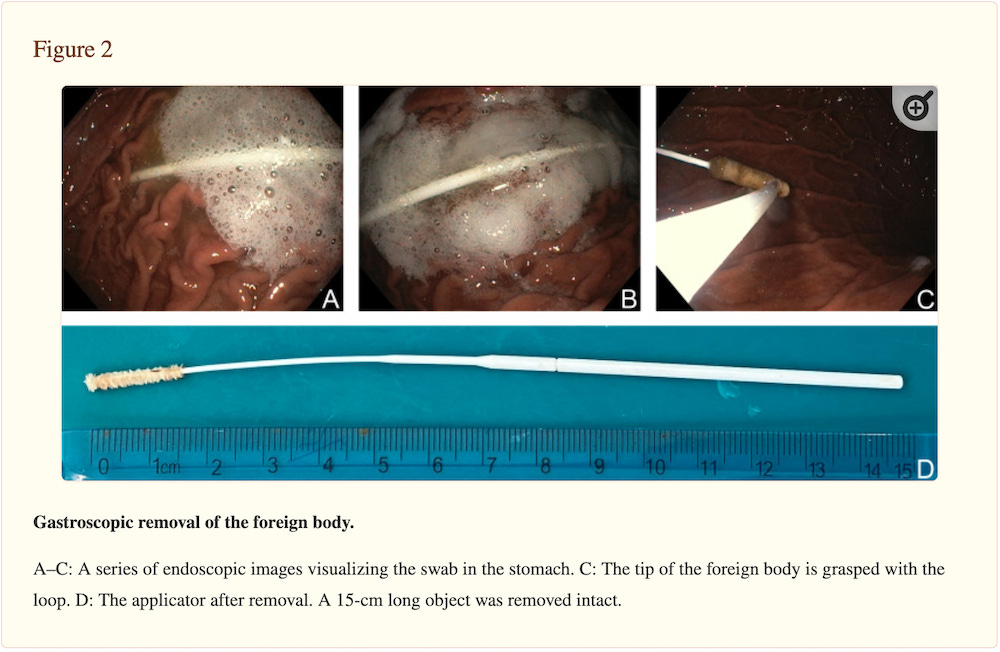
Safety Precautions for Self-Performed Severe Acute Respiratory Syndrome Coronavirus 2 Tests: A Case of a Swallowed Swab
A 45-year-old male patient arrived at our otorhinolaryngology department for an emergency examination. Owing to the policy of his employing company, he was obliged to self-test for SARS-CoV-2 twice a week. Four hours before his arrival, the patient had attempted to perform a SARS-CoV-2 rapid antigen test (GenBody Inc, Cheonan, KR) at home by taking an OPS. Upon specimen collection, he felt a mild resistance and had a gag reflex, which resulted in the ingestion of the swab applicator.
In collaboration with the department of gastroenterology, we performed an urgent gastroscopy with a flexible endoscope (Olympus, JP). Despite four hours having elapsed since the incident, we still identified the swab stick intact in the stomach. After firmly catching the object with a polypectomy loop, it was withdrawn and removed safely. A second look showed no signs of mucosal damage or any residual foreign bodies along the esophagus and stomach. We examined the foreign body and confirmed that it had been removed without missing parts.
August 4, 2021
Case Report: An Intracranial Complication of COVID-19 Nasopharyngeal Swab
A 54-year-old female with diagnosed CSF leak presented to the emergency department (ED) with acute onset of severe headache, and neck and back pain. Prior to this presentation, the patient had experienced two months of persistent headache and rhinorrhea since her coronavirus disease 2019 (COVID-19) nasopharyngeal swab. As part of her outpatient workup, an otolaryngology consultation with subsequent beta-2 transferrin testing and magnetic resonance imaging was performed and she was diagnosed with a CSF leak from ruptured congenital meningocele. On ED presentation, she was afebrile, but with mild tachycardia, leukocytosis, and meningismus. Lumbar puncture revealed acute streptococcal meningitis. This patient’s meningitis developed due to prolonged occult CSF leak after her COVID-19 nasopharyngeal swab ruptured a pre-existing congenital meningocele.
Conclusion
Nasopharyngeal swabs are being performed much more frequently due to the COVID-19 pandemic. All front-line providers should be aware of the potential presence and rupture of congenital meningoceles in patients who have undergone recent nasopharyngeal swab when risk-stratifying for potential CSF leak and meningitis.
September 9, 2021
Cribriform Plate Injury After Nasal Swab Testing for COVID-19
An otherwise healthy man in his 40s presented for right-sided clear water rhinorrhea in December of 2020. Rhinorrhea originated after nasal swab testing and was mistakenly considered to be allergic rhinitis in the patient. The test was performed by a mobile unit at the patient’s home in March of 2020. The test was indicated because of previous contact with a woman who had a positive COVID-19 test result 5 days earlier. The patient had no symptoms of COVID-19 infection and RNA of SARS-CoV-2 was not detected by polymerase chain reaction (PCR) testing.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2784128
September 19, 2021
CT reveals shocking injury caused by COVID-19 nasal swab
The man, who had no previous injury to his skull and was otherwise healthy, underwent COVID-19 testing after being in contact with a woman who had tested positive for SARS-CoV-2. He had no COVID-19 symptoms, and his polymerase chain reaction (PCR) test result was negative.
An analysis of the patient's nasal discharge showed a high level of the beta-trace protein (23.7 mg/L) in the nasal secretion (normal range < 6 mg/L). The beta-trace protein test is a quick, noninvasive, and inexpensive method to detect CSF fluid in nasal secretions.
"Every instance of unilateral clear water rhinorrhea that appears after transnasal testing must be considered a potential CSF leak," the team wrote.
A brief report: Cerebrospinal fluid rhinorrhea after repetitive nasal swab testing for coronavirus disease 2019(COVID-19)
A 47-year-old male was admitted with a right-sided rhinorrhea and headache. The patient had been tested for COVID-19 four times within the span of the previous month. Following the first swab test, the patient reported some minor fluid leak from his right nasal cavity. Three days after the last nasal swab test, the dripping developed into massive fluid leak following a sneeze.
The physical examination showed leakage of a clear fluid from the right nasal cavity. We have suspected a [CerebroSpinal Fluid] CSF leak due to the fluid's characteristics and amount.
The patient was admitted to the hospital for an endoscopic transnasal surgery. During the surgery, a bone defect was identified at the right fovea ethmoidalis. The defect was repaired with synthetic dura mater and was supported with a nasoseptal flap.
https://www.sciencedirect.com/science/article/pii/S2468548821000539
October 9, 2021
CSF rhinorrhea after nasopharyngeal swab testing for COVID-19: A case report and review of literature
A 47 years old woman presented with unilateral rhinorrhea on the right, progressive headache, and photophobia from a week ago. The patient had recently taken Covid-19 nasopharyngeal swab test as she had contact with a positive Covid-19 patient. Shortly after, she experienced rhinorrhea accompanied by a headache. She had no history of similar symptoms before. Her medical history was also negative for any types of surgery and illnesses. In physical examination, she had no abnormal findings other than clear rhinorrhea from the right side. The drained fluid was positive for beta-2 transferrin, proving that her rhinorrhea was caused by a CSF leakage.
She was enlisted for an endoscopic surgical repair of the defect. During the operation, the defect was sealed using fat and fascia lata. The patient's ICP was measured two weeks and four weeks after the operation and was normal in both cases. In a follow-up visit two months after surgery, the patient was good and did not have any complaints.
OCTOBER 25, 2021
Iatrogenic cerebrospinal fluid leak after repeated nasal swab tests for COVID-19: illustrative case
A 41-year-old man presented with clear continuous rhinorrhea through his left nostril for 5 days after repeated nasal swabbing for COVID-19. There were no obvious risk factors for spontaneous CSF leak. Computed tomography cisternography showed contrast accumulation in the left olfactory fossa and along the left nasal cavity. Such findings aligned with a preliminary diagnosis of CSF leakage through the left cribriform plate. Magnetic resonance imaging confirmed the presence of a CSF fistula between his left cribriform plate and superior nasal concha. The patient underwent endoscopic endonasal repair. CSF rhinorrhea ceased after the surgery, and no recurrence was noted during the 12-week postoperative follow-up period.
Although rare, iatrogenic CSF leakage can be a serious complication following COVID-19 nasal swab tests, especially when infection may cause significant neurological sequelae.
https://thejns.org/caselessons/view/journals/j-neurosurg-case-lessons/2/17/article-CASE21421.xml
November 12, 2021
How deep is too deep? Gastrointestinal complication of COVID-19 deep nasal swab testing
We present the case of a 35-year-old woman at 40 weeks gestation who presented to the hospital for a scheduled elective induction and delivery for full-term pregnancy. On admission, she underwent routine testing for COVID-19 with deep nasal swab. The swab was inserted into her left naris, and while being rotated, broke off at the indicator line in the patient’s posterior nasopharynx. Almost immediately, the patient felt pain in her throat that quickly subsided. Because the swab tip was lost, the patient underwent a second uneventful COVID-19 deep nasal swab, which was negative.
The patient’s induced labor continued because the distal nasal swab tip was thought to be lodged in the nasopharynx. However, a stat x-ray and urgent laryngoscopy did not show the location of the swab. After experimenting by breaking similar COVID-19 swabs, it was determined that the broken plastic from the distal swab appeared to be sharp. Therefore, endoscopy was planned to locate and retrieve the swallowed swab tip. Following delivery of a healthy neonate, the patient underwent push enteroscopy 8 hours after suspected ingestion. Endoscopy demonstrated a normal esophagus, stomach, and proximal duodenum with no evidence of prior trauma. The broken swab was then located in the fourth portion of the duodenum. Using raptor forceps, the swab tip was oriented vertically to safely grasp the sharp end. The swab tip was carefully removed with only mild gastric mucosal trauma on retrieval. The retrieved swab tip was compared to the broken swab shaft to confirm complete extraction.
November 13, 2021
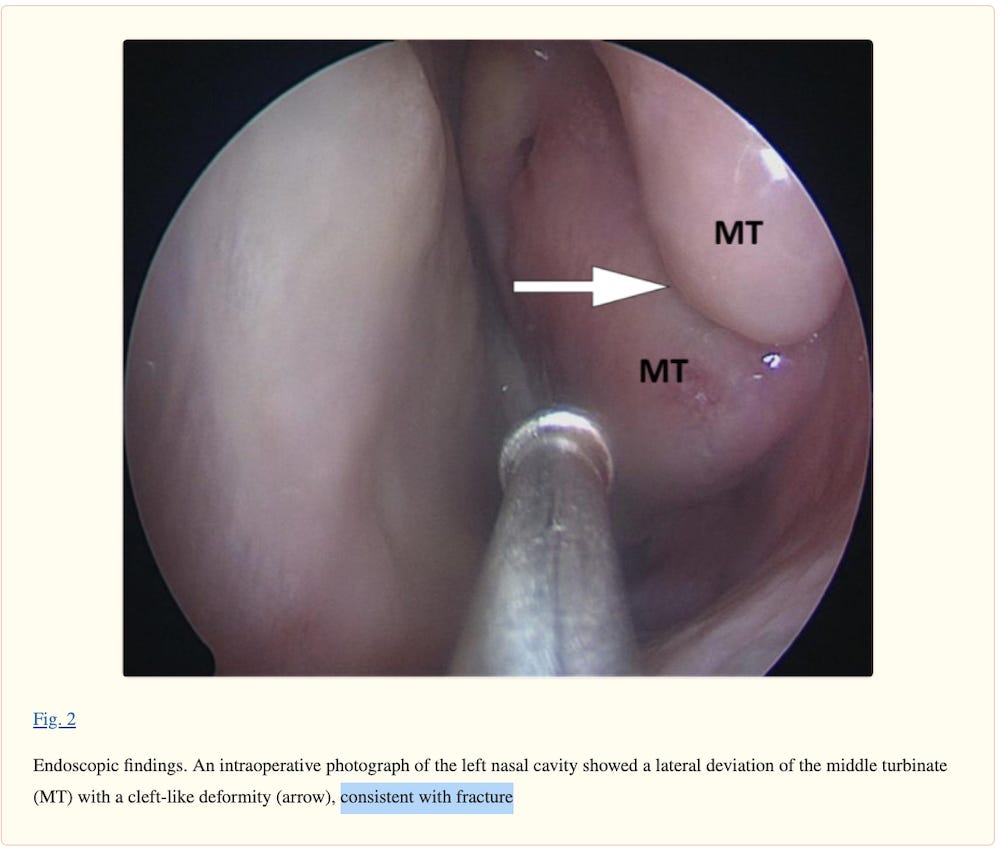
Ethmoidal silent sinus syndrome after nasal swab test
A healthy male in his 40s presented with a 3-month history of frontal headache and post-nasal drip, which did not improve with oral antibiotics. One month prior to the onset of the symptoms, he underwent a nasopharyngeal swab testing for SARS-CoV-2 (which yielded a negative result) for a history of malaise and cough. The patient claimed that the swab insertion into the nasal cavity was particularly painful on the left side. He denied any history of facial trauma, nasal surgery, or chronic sinusitis, and his medical history was unremarkable.
Sinus computed tomography (CT) scan showed a lateral deviation of the left middle nasal turbinate. The patient was diagnosed with ethmoid silent sinus syndrome. He was admitted to the hospital for endoscopic surgical repair. Intraoperative endoscopy revealed that the left middle turbinate was laterally deviated, with an umbilication-like deformity in its middle third. The findings were consistent with a fracture, and it was likely related to the nasopharyngeal swab testing performed 1 month before the onset of symptoms.
November 15, 2021
Cerebrospinal Fluid Leak From COVID-19 Swab
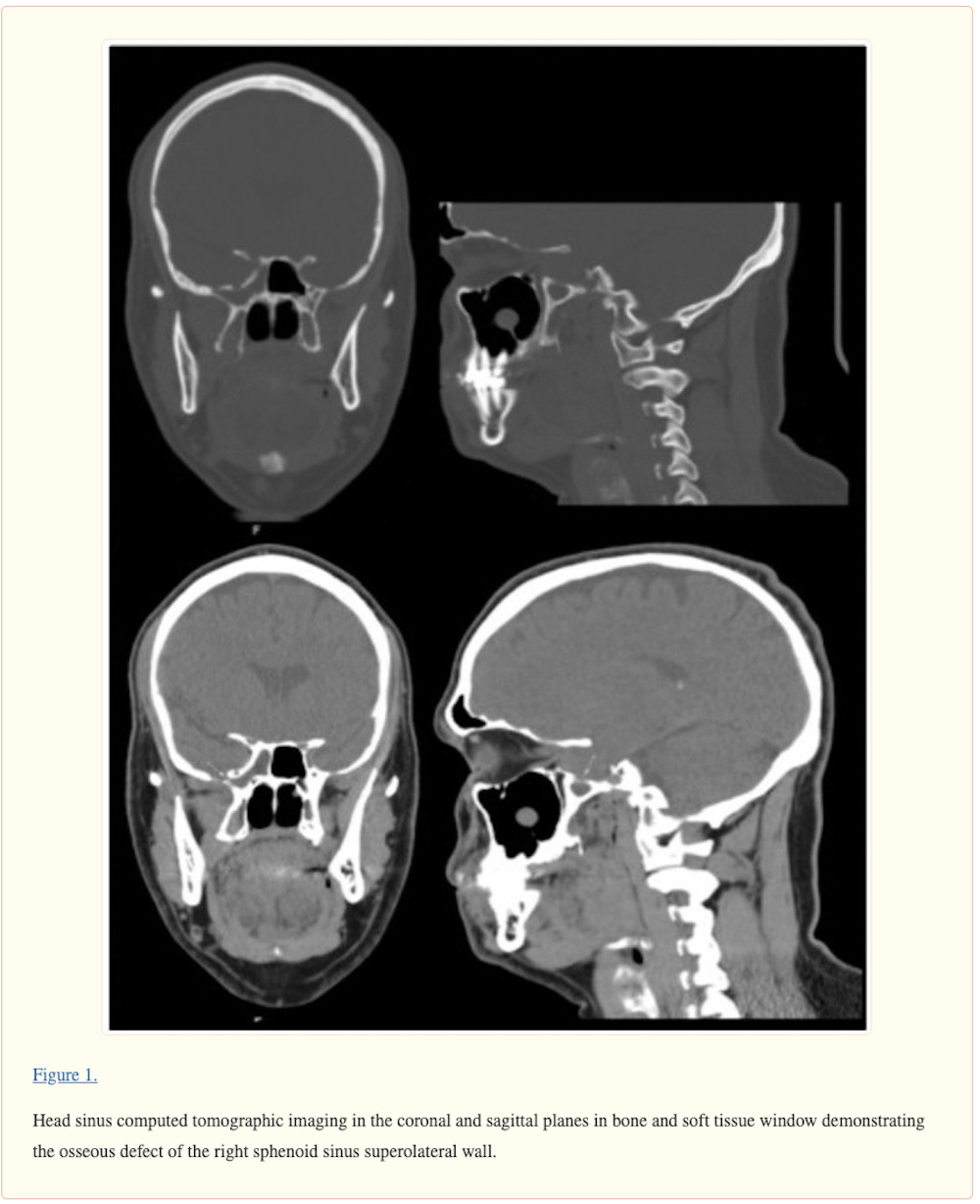
A 40-year-old man presented to the clinic for evaluation of CSF leak following COVID-19 testing via nasopharyngeal swab. During the swab, the patient reported feeling “something crack” upon deeper insertion of the swab and then had a large amount of clear rhinorrhea. Since the COVID-19 test, the patient had persistent clear fluid drain from the right side of his nose when tilting his head forward. The clear fluid was positive for beta-2 transferrin, and head computed tomographic imaging showed a small osseous defect in the superior and lateral wall of the right sphenoid sinus with opacification. The patient had resolution of CSF leak following repair of right skull base defect by an endoscopic transnasal/transsphenoidal approach with nasoseptal flap.
November 18, 2021
Must This Swab Go That Far Up Your Nose to Test for Covid?
One Canadian said it felt like a painful poke to his brain. An American heard crunching sounds in her head. A Frenchwoman suffered a severe nosebleed. Others got headaches, cried or were left in shock.
They were all tested for Covid-19 with deep nasal swabs.
“It felt like someone was going right into the reset button of my brain to switch something over,” Paul Chin, a music producer and DJ in Toronto, said of his nasal swab test. “There’s truly nothing like it.”
December 3, 2021
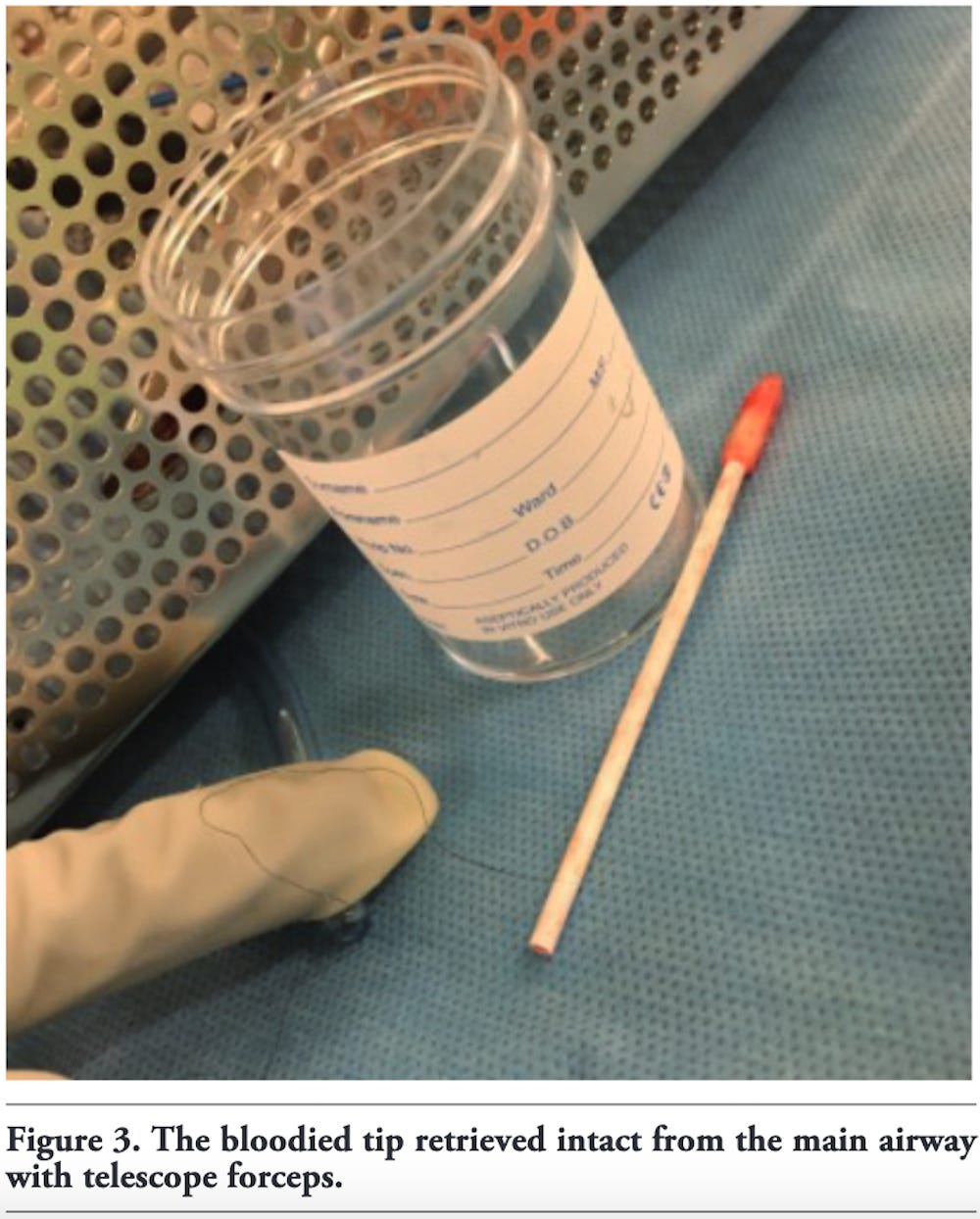
A challenging case of tracheal foreign body retrieval following COVID-19 swabbing
A 35 year-old female patient with multiple co-morbidities was admitted to the intensive care unit (ICU) and ultimately required intubation and tracheostomy formation for ventilatory wean. Several failed extubation attempts demanded an in-patient assessment of the airway under anesthetic. Microlaryncoscopy and rigid bronchoscopy identified sub-glot-tic stenosis from granulation and scar tissue which was excised at the time of surgery. She was stepped down from ICU to a specialist ear, nose, and throat (ENT) ward after 120 days with a focus on rehabilitation due to significant deconditioning. Due to further failed de-cannu-lation attempts, discharge with a long-term tracheostomy was planned, with further airway procedures to be considered when fully recovered as an out-patient.
Nine days after step-down, the patient was routinely swabbed for the virus by a registered nurse. For unclear reasons, the swab was done via the tracheostomy inner cannula and not via the nose or throat. This was not established procedure within our trust. As the swab was inserted in to the tracheostomy it snapped at the break point, with the tip falling through the inner tube. It was not visible on immediate inspection. This caused the patient to cough with episodic desaturation. High flow oxygen was administered as well as nebulized adrenalin.
The patient was taken to theatre and under general ansesthetic a flexible bronchoscope with grabbing forceps was introduced via the tracheostomy. The swab was seen once again but attempts to remove it failed and resulted in worsening airway oedema as reported by the ENT team. The procedure was abandoned and further nebulized adrenaline and intravenous corticosteroids were administered. A chest radiograph was taken that evening and there was no evidence of pneumothorax or lobar collapse and the swab tip – as expected – was not visible.
The patient was subsequently referred to our team which has experience in complex large airway intervention. She under-went rigid and flexible bronchoscopy under a second general anaesthetic the following day. Due to significant subglottic steno-sis the rigid bronchoscope was inserted directly via the tra-cheostomy stoma in the neck. The swab tip was visualized in the right main bronchus with the proximal end closely applied to the lateral tracheal wall. It was successfully removed with telescope forceps under direction visualisation. The retrieved tip measured approximately 5cm. There was evidence of generalized airway oedema and associated oozing immediately following removal.
https://www.monaldi-archives.org/macd/article/view/2014/1371
March 21, 2022
Complications of Nasopharyngeal Swabs and Safe Procedures for COVID-19 Testing Based on Anatomical Knowledge
Patients and clinicians should be aware of rare but possible complications and associated high-risk factors.
The PubMed and Embase databases were searched for articles published between 2019 and 2022. KoreaMed was explored between 2010 and 2022 due to the relative shortage of products in the pilot search. The searched keywords included “nasopharyngeal swab,” “nasopharynx swab,” “nasal swab,” “pernasal swab,” “rhinopharyngeal swab,” “pharyngeal swab,” “nasopharyngeal test,” “swab stick,” “swabbing test,” “complications,” “safe,” “safety,” “COVID,” “severe acute respiratory syndrome,” “coronavirus,” “2019nCoV,” “nCoV2019” or “HCoV-19,” and “NCOVID-19”. The literature search focused on human studies and excluded animal experiments.
Retained swabs 3, 12, 16, 17, 18, 20, 21, 24, 26, 27, 32, 35 due to swab fracture during the examination and epistaxis [nosebleed] 3, 12, 17, 24, 28, 32 were the frequently reported complications.
Cerebrospinal fluid (CSF) leakage 3, 11, 12, 15, 22, 23, 28, 29, 30, 33, 34, 36 was a frequently documented serious adverse event requiring prompt attention and evaluation.
Nasal septal abscess, 3, 12, 17, 19, 25 and ethmoidal silent syndrome 31 were also reported as related complications after nasopharyngeal swabbing.
July 18, 2022
Lawsuit: ‘Violent’ COVID nasal swab ruptured patient’s sinus cavity
Please read the articles below:
IATROGENESIS:
Any adverse effect (or complication) resulting from medical treatment.
PROTECT YOURSELF
James Roguski
310-619-3055
JamesRoguski.substack.com/archive
All content is free to all readers.
All support is deeply appreciated.




































As horrible these are to READ, and in my viewpoint and experience that this is a tortuous procedure, to millions more that are not reported, I will again say God Bless you James for the OUTSTANDING humanitarian work you have done.
May angels watch over you!
Here is a chain of logic: Masks were mandated because covid was spread from aerosolized saliva secretions. Therefore saliva must contain the virus in order to be an infectious agent. Therefore testing saliva would yield confirmation of infection if there was any. Therefore testing saliva would be sufficient in and of itself... no need for a nasal swab and certainly no need to shove a swab up to the limit of the nasal cavity. Was there an alternative purpose for this invasive swab?